Anaphylaxis Symptom Checker
Is this anaphylaxis?
Based on symptoms reported, this tool helps determine if you or someone else might be experiencing medication-induced anaphylaxis. Anaphylaxis is a life-threatening emergency requiring immediate action.
Epinephrine Dose: Inject 0.3-0.5 mg into outer thigh (hold 10 seconds)
Repeat every 5-15 minutes if symptoms don't improve
Immediate Actions:
- Administer epinephrine immediately
- Call emergency services (911)
- Stay with the person until help arrives
- Lay flat unless breathing is difficult
When a medication triggers a severe allergic reaction, it doesn’t wait for permission. It strikes fast-sometimes in under a minute. Your skin breaks out in hives. Your throat tightens. Your blood pressure drops. You can’t breathe. This isn’t just a bad reaction. This is anaphylaxis, and it can kill you if you don’t act immediately.
What Anaphylaxis Really Looks Like
Anaphylaxis isn’t a rash or a stomachache. It’s a full-body emergency. The body’s immune system goes into overdrive, releasing chemicals that cause blood vessels to leak, airways to swell, and the heart to struggle. Medications are one of the top causes-responsible for about 15% of all anaphylaxis cases in the U.S. According to the CDC, around 38,200 people visit emergency rooms each year because of a drug-triggered reaction. The signs don’t always show up the same way. But there are clear patterns. Most reactions happen within 5 to 30 minutes after taking the drug, especially if it’s given through an IV. Oral meds might take a bit longer-up to an hour or even six hours in rare cases. Here’s what to watch for:- Skin: Hives, itching, flushing, swelling of lips, tongue, or throat
- Respiratory: Wheezing, shortness of breath, tight chest, hoarse voice, feeling like you’re choking
- Circulatory: Dizziness, fainting, rapid or weak pulse, low blood pressure
- Gastrointestinal: Nausea, vomiting, cramps, diarrhea
- Skin symptoms + trouble breathing or low blood pressure
- Two or more systems affected (skin + gut, or skin + breathing, etc.)
- Low blood pressure alone after taking a known allergen
Which Medications Are Most Likely to Trigger It?
Not all drugs carry the same risk. Some are far more dangerous than others. Antibiotics are the biggest culprit-accounting for nearly 70% of all medication-induced anaphylaxis. Penicillin and its cousins (like amoxicillin) are the most common offenders. If you’ve ever had a rash after taking penicillin, you’re not just “sensitive.” You could be at risk for a life-threatening reaction next time. NSAIDs like ibuprofen and naproxen are next on the list. These are common, over-the-counter drugs, but they can trigger anaphylaxis even in people who’ve taken them safely for years. That’s because they don’t always work through the same immune pathway as antibiotics. Sometimes, it’s not IgE-mediated-it’s a direct chemical reaction that mimics anaphylaxis. Monoclonal antibodies-used in cancer and autoimmune treatments like rituximab or cetuximab-are also high-risk. These are newer drugs, and their use is growing fast. That’s why the FDA now requires stronger warning labels on them. Even contrast dye used in CT scans can cause reactions. Many people think it’s “just an allergy to dye,” but it’s often a true anaphylactic response. And it’s not always preventable-even with premedication.Why Medication Reactions Are More Dangerous Than Food Reactions
Food allergies cause more anaphylaxis overall-but drug reactions are deadlier. Why? In food reactions, symptoms usually start with itching or hives. People recognize it early. They stop eating, grab their epinephrine, and act. With medications, it’s different. You’re in a hospital, clinic, or pharmacy. You’re being monitored. You assume someone else is watching. So when your blood pressure drops, the nurse thinks it’s a vasovagal response. When you start wheezing, they think it’s anxiety or asthma. When your face swells, they think it’s a reaction to the IV line. A 2022 JAMA study found that medication-induced anaphylaxis has nearly triple the death rate of food-triggered cases. Why? Because it’s missed. And when it’s missed, epinephrine is delayed-or never given at all. A 2023 review in the Annals of Allergy, Asthma & Immunology found that 78% of fatal cases involved delayed or missing epinephrine. In 34% of cases, no epinephrine was given at all.Epinephrine Is the Only Lifesaver
There’s no other treatment that works like epinephrine. Antihistamines? They help with itching. Steroids? They reduce swelling later. But only epinephrine stops the cascade that kills you. It tightens blood vessels to raise blood pressure. It opens airways. It calms the immune system’s explosion. The timing matters. The American Heart Association says epinephrine must be given within 5 to 15 minutes of symptom onset. After 30 minutes, the risk of death jumps by 300%. How to use it:- Inject into the outer thigh-through clothing if needed
- Hold for 10 seconds
- Dose for adults: 0.3 to 0.5 mg (standard auto-injector)
- You can repeat it every 5 to 15 minutes if symptoms don’t improve
What Gets Mistaken for Anaphylaxis
Not every bad reaction is anaphylaxis. Some look the same but aren’t. Misdiagnosing them leads to unnecessary panic-or worse, missed treatment. “Red man syndrome” from vancomycin is one example. It causes flushing, itching, and rash-like an allergic reaction. But it doesn’t cause low blood pressure or breathing trouble. It’s caused by too-fast IV infusion, not an immune response. Slowing the drip fixes it. Other mimics:- Panic attacks (rapid breathing, dizziness, tingling)
- Pulmonary embolism (sudden shortness of breath, chest pain)
- Sepsis (fever, low BP, confusion)
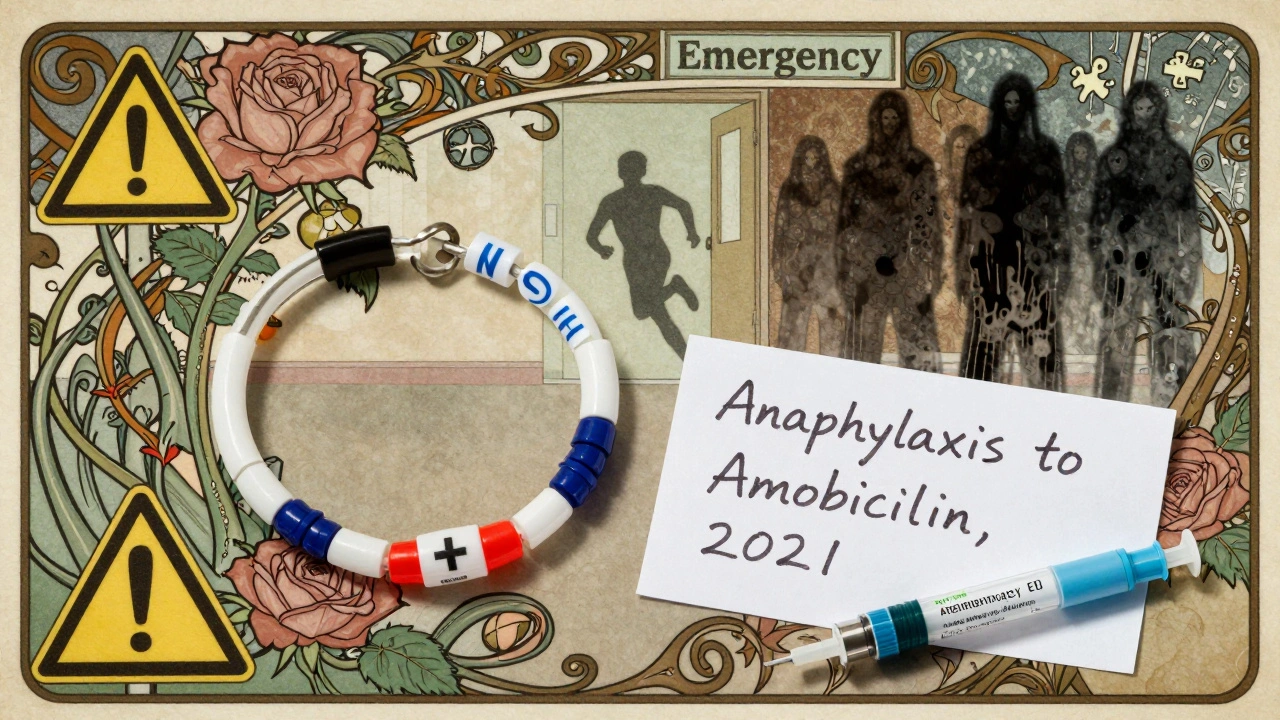
How to Prevent It
Prevention starts with accurate records. If you’ve ever had a reaction to a drug, write it down. Not just “allergic to penicillin.” Say: “Anaphylaxis to amoxicillin in 2021-swelling, trouble breathing, epinephrine required.” Too many people say, “I had a rash once.” That’s not enough. Anaphylaxis is not a rash. It’s a near-death experience. Hospitals are getting better. Johns Hopkins cut anaphylaxis incidents by 47% after adding an automated allergy alert system to their electronic records. But 63% of medication errors still happen because allergy info is missing or vague in EHRs. If you’ve had anaphylaxis before:- Carry two epinephrine auto-injectors at all times
- Wear a medical alert bracelet
- Get a referral to an allergist for testing
- Ask for a written anaphylaxis action plan
What Comes After
Surviving anaphylaxis isn’t the end. It’s the beginning of a new normal. You’ll need follow-up testing. Skin prick tests or blood tests (like IgE testing) can confirm what caused it. The FDA approved a new rapid test for penicillin allergy in June 2023-it gives results in 15 minutes with 93% accuracy. Some people can be desensitized. If you need a drug you’re allergic to-like chemotherapy or a life-saving antibiotic-specialized clinics can slowly introduce tiny doses under close supervision. It’s risky, but it works. And you need to educate everyone around you. Your family. Your coworkers. Your pharmacist. If you collapse, they need to know what to do. Don’t assume they’ll know what epinephrine is. Show them how to use the injector. Practice with a trainer device.The Bottom Line
Anaphylaxis from medications is rare-but deadly. It doesn’t care if you’re healthy, young, or have never had an allergy before. It strikes fast, and it strikes silently. The good news? It’s preventable. It’s treatable. But only if you know the signs-and act before it’s too late. If you’ve ever had a bad reaction to a drug-even if it was “just a rash”-talk to your doctor. Get tested. Get an epinephrine injector. Write it down. Tell people. Because next time, you might not be so lucky.Can you survive anaphylaxis without epinephrine?
Surviving anaphylaxis without epinephrine is possible-but extremely rare and dangerous. Epinephrine is the only medication that reverses the life-threatening symptoms: airway swelling, low blood pressure, and shock. Without it, the body’s reaction continues unchecked. Studies show that delays beyond 30 minutes increase the risk of death by 300%. Many fatal cases involve no epinephrine at all. Antihistamines and steroids may help with milder symptoms, but they do not stop the collapse of the cardiovascular system. Epinephrine is not optional-it’s essential.
Can you develop anaphylaxis to a medication you’ve taken before without problems?
Yes. Anaphylaxis can happen the first time you take a drug-or the 50th. Your immune system doesn’t always react immediately. Sometimes, it takes multiple exposures to become sensitized. Antibiotics like penicillin and NSAIDs like ibuprofen are common triggers for delayed reactions. Even if you’ve taken the same medication for years without issue, your body can suddenly start treating it as a threat. That’s why doctors always ask about past reactions-even if you say you’ve never had one.
Is anaphylaxis from medications more dangerous than food-induced anaphylaxis?
Yes, medication-induced anaphylaxis has a higher death rate-nearly 1.8% compared to 0.7% for food-triggered cases. Why? Because it’s often missed. In hospitals and clinics, symptoms like low blood pressure or wheezing are frequently mistaken for side effects, anxiety, or procedural complications. People don’t recognize it as an allergic emergency until it’s too late. Also, many medications are given intravenously, which causes faster, more intense reactions. Food reactions usually start with itching or hives, which are easier to notice and act on quickly.
What should I do if I think someone is having anaphylaxis from a medication?
Act immediately. First, give epinephrine into the outer thigh-even through clothing. Use the auto-injector and hold it for 10 seconds. Call emergency services right after. Lay the person flat, unless they’re having trouble breathing-in which case, let them sit up. Do not give them anything to drink. Do not wait for symptoms to worsen. Do not assume it’s just anxiety or a panic attack. Epinephrine is safe to use even if you’re unsure. If symptoms don’t improve in 5-15 minutes, give a second dose. Stay with them until help arrives.
Do I need to carry epinephrine if I’ve only had a mild reaction before?
Yes. Even a mild reaction-like hives or swelling-is a warning sign. Studies show that people who’ve had any allergic reaction to a medication are at higher risk for a severe one next time. Anaphylaxis can escalate quickly. A rash today could mean throat closure tomorrow. The American Academy of Allergy recommends that anyone with a history of any allergic reaction to a drug should carry two epinephrine auto-injectors. Don’t wait for a near-death experience to take it seriously.
Can anaphylaxis be cured?
Anaphylaxis itself isn’t a disease-it’s a reaction. You can’t “cure” it, but you can manage the risk. For some drugs, like penicillin, allergy testing can confirm whether you’re truly allergic. If you are, avoiding the drug is the best protection. In some cases, especially with chemotherapy or antibiotics you absolutely need, doctors can perform desensitization: slowly introducing tiny doses under strict supervision. This can allow you to safely receive the drug again. But once you’ve had anaphylaxis, you’ll always need to be cautious. Carry epinephrine. Wear a medical alert. Always tell healthcare providers.


14 Comments
Just had my first epinephrine auto-injector refill last week. Been carrying two since my amoxicillin incident in 2019. People think it’s overkill until they see your face swell up in a pharmacy. Don’t wait for a near-death experience. Get it. Know how to use it. Teach your damn family. 🇦🇺
It’s wild how we treat meds like they’re harmless candy. We’ll check the expiration on our yogurt but not ask if that antibiotic could kill us. Anaphylaxis isn’t rare-it’s silent. And the real tragedy isn’t the reaction-it’s how often we miss it because we’re trained to look for something else. We need better protocols, not just better awareness.
Wait… so are you saying the government is hiding the truth about vaccines causing anaphylaxis?? 😳 I read this one guy on TruthTube who said the FDA knows 87% of reactions are from mRNA adjuvants but they cover it up to keep pharma profits rolling 💉🩸 #WakeUpSheeple
While the clinical guidance presented herein is both accurate and commendable, I would respectfully submit that the omission of pharmacokinetic variables in the context of polypharmacy remains a significant gap in public education. For geriatric patients, the delayed clearance of NSAIDs in conjunction with ACE inhibitors may potentiate hypotensive episodes that mimic anaphylaxis, thereby confounding diagnostic fidelity. Further research into biomarker differentiation is warranted.
Man, I used to think I was just "sensitive" to ibuprofen-got a little rash once, didn’t think twice. Then my buddy had a full-blown reaction after a single Advil at a concert. He was down for 12 minutes before they got the epinephrine in. I carry two now. I made my wife memorize the steps. I even bought a trainer pen and let my 7-year-old practice on a banana. 🍌💉 You think it won’t happen to you? It already did. You just didn’t know it yet.
Everyone’s acting like this is some groundbreaking revelation. Newsflash: doctors have been screwing this up for decades. I’ve been to three ERs where they gave me Benadryl instead of epinephrine. One nurse even said, "It’s probably just anxiety." My throat closed. My blood pressure crashed. I almost died because they didn’t know the difference between a rash and a death sentence. And now we’re just going to tell people to "get tested"? What about the ones who can’t afford an allergist? What about the ones who don’t have insurance? This isn’t a checklist-it’s a systemic failure.
I’m so glad this was written. I had a reaction to a tetanus shot last year and no one took it seriously. I just cried and said "I think I’m dying" and they gave me a soda. 😔 I didn’t tell anyone because I felt stupid. But now I carry two injectors and wear my bracelet every day. I even made a little card for my coworkers. You’re not overreacting if your body says you’re dying. You’re just finally listening.
Let’s be real: the only reason this is getting attention is because it’s not food-related. If this were about peanuts or shellfish, we’d have mandatory labeling, public awareness campaigns, and a damn national holiday. But because it’s pills and IVs? It’s just "medical stuff." Meanwhile, people are dying in hospitals because nurses think "low BP = dehydration." Wake up. This isn’t a rare side effect-it’s a murder by neglect.
Okay, imagine your immune system is a hyperactive toddler with a flamethrower. You hand it a pill-"Here, sweetie, take this!"-and boom. Fireworks. The toddler doesn’t care if you’ve taken it 20 times before. It just saw a new toy and went full nuclear. Now the ER is a warzone: wheezing like a broken accordion, skin glowing like a neon sign, blood pressure flatlining. And the only thing that stops it? A 0.3mg shot of adrenaline. Not a prayer. Not a tea. Not a hug. A needle. And you better know where to aim.
epi pen > everything. i had a rash once. now i carry two. my wife knows how to use it. my dog even knows the sound. no excuses. just do it.
I’ve been on 12 different meds in the last 5 years and never had a reaction. But I still carry two epinephrine pens because I don’t want to be the person who says "I didn’t think it would happen to me" while my family watches me turn blue. I don’t care if you think it’s paranoid. I care that I’m alive. And if you’re not carrying one, you’re playing Russian roulette with your own body. I’m not mad. I’m just disappointed.
bro why are we even talking about this like its a big deal. i took penicillin 3 times and only got a little rash. now i got a new job and they want me to get a physical and they asked if i was allergic and i said "maybe" and they said "oh cool" and gave me a shot anyway. i was fine. stop fearmongering.
This is an excellent, meticulously researched overview. I particularly appreciate the emphasis on distinguishing true anaphylaxis from pharmacological mimics like red man syndrome. The data on delayed epinephrine administration is sobering. I’d only add that in institutional settings, standardized anaphylaxis response protocols-paired with mandatory staff drills-could reduce mortality by up to 60%. This isn’t just patient education; it’s systems-level reform.
Richard, you’re right about systems. My hospital just rolled out an automated alert that pops up if you type "penicillin" in the EHR. It forces you to pick from three options: "allergic," "non-allergic," or "unknown." No more "mild rash once" as a free-text answer. It’s small, but it’s something. We’re getting there.