Antihistamine Side Effect Risk Calculator
Select Your Antihistamine Type
Choose the type of antihistamine you're taking to see side effect risks
Side Effect Comparison
| Side Effect | First-Generation | Second-Generation |
|---|---|---|
| Dry Mouth | 28% | 2-4% |
| Constipation | 15-20% | 3-5% |
| Urinary Issues | 5-8% | <1% |
| Cognitive Risk | 54% higher dementia risk | Minimal risk |
Dementia Risk Assessment
Warning: Each extra year of use beyond 90 daily doses increases dementia risk by 20%.
Recommended Alternatives
Safer Alternatives
Second-generation antihistamines have minimal anticholinergic effects:
- Cetirizine (Zyrtec)
- Loratadine (Claritin)
- Fexofenadine (Allegra)
- Levocetirizine
Important Tips
Avoid combining with other anticholinergics:
- Check medication labels for "PM" or "nighttime" formulas
- Avoid if you have enlarged prostate or glaucoma
- Never combine with other anticholinergic drugs
- Consider non-drug alternatives for sleep: melatonin or humidifiers
Many people reach for antihistamines like Benadryl for allergies, colds, or even sleep. But what they don’t realize is that these common pills come with hidden side effects that can seriously affect daily life-dry mouth, constipation, trouble peeing, and even brain fog. These aren’t just minor annoyances. They’re signs of something deeper: anticholinergic effects.
What Are Anticholinergic Effects?
Anticholinergic effects happen when a drug blocks acetylcholine, a chemical in your body that tells muscles and glands what to do. Most antihistamines are designed to block histamine, which causes allergy symptoms. But first-generation antihistamines-like diphenhydramine, chlorpheniramine, and promethazine-also accidentally block acetylcholine receptors. This is like turning off a switch you didn’t mean to touch. These drugs were developed in the 1940s, and back then, nobody thought much about the side effects. Today, we know better. The same mechanism that makes you drowsy also slows down your saliva, gut, and bladder. And while second-generation antihistamines like cetirizine (Zyrtec), loratadine (Claritin), and fexofenadine (Allegra) were designed to avoid this, first-generation ones are still widely available, cheap, and often taken without thinking.Dry Mouth: More Than Just Uncomfortable
If you’ve ever felt like your mouth is full of cotton after taking Benadryl, you’re not imagining it. Anticholinergic drugs cut saliva production by 60-70%. That’s not just inconvenient-it’s dangerous. Saliva doesn’t just help you swallow. It protects your teeth, washes away bacteria, and keeps your mouth from getting infected. Without enough of it, you’re at higher risk for cavities, gum disease, and oral thrush. People who take these meds regularly often end up drinking water constantly, chewing gum, or using saliva substitutes. Sugar-free gum with xylitol can boost saliva flow by 40-60% within minutes, according to the American Dental Association. But that’s just treating the symptom, not the cause.Constipation: When Your Gut Slows Down
Your gut moves food along thanks to rhythmic muscle contractions controlled by acetylcholine. When antihistamines block that signal, your bowels slow down. Studies show transit time increases by 1.5 to 2 times normal. That means food sits longer, water gets sucked out, and stools become hard and difficult to pass. About 15-20% of people taking first-generation antihistamines report constipation. For older adults or those already prone to bowel issues, this can lead to serious complications-fecal impaction, bowel obstruction, or even hospitalization. The American Gastroenterological Association recommends taking a daily stool softener like polyethylene glycol (17g) if you must use these meds. It cuts constipation risk from 18% down to 5% in clinical trials.Urinary Issues: More Than Just a Nuisance
Bladder function relies on acetylcholine to contract the detrusor muscle and empty urine. When antihistamines block this, the bladder can’t squeeze properly. At the same time, the urethral sphincter tightens, making it harder to start peeing. The result? Urinary retention. This isn’t just about needing to go more often. It’s about not being able to go at all. In men with enlarged prostates, first-generation antihistamines can trigger acute urinary retention within 48 hours. The American Urological Association warns against using these drugs in men with prostate symptom scores above 8. For women, especially older ones, this can mean frequent urinary tract infections or the need for catheterization.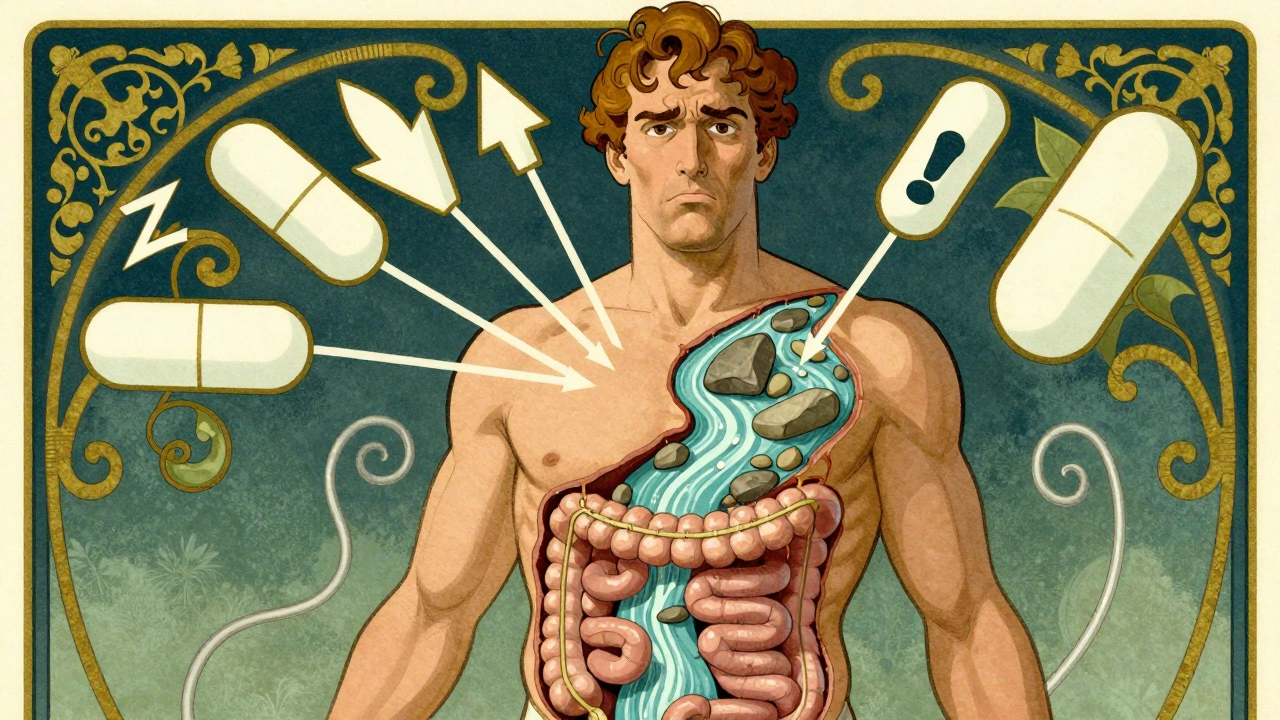
Why First-Generation vs. Second-Generation Matters
Not all antihistamines are the same. First-generation ones cross the blood-brain barrier easily. That’s why they make you sleepy. But it’s also why they cause strong anticholinergic effects. Diphenhydramine has a Ki value of 87 nM for muscarinic receptors-meaning it binds tightly and blocks acetylcholine effectively. Second-generation antihistamines like fexofenadine and loratadine barely touch those receptors. Their Ki values are over 1,000 nM. That means at normal doses, they’re practically invisible to acetylcholine receptors. The numbers don’t lie:- Dry mouth: 28% with diphenhydramine vs. 2-4% with second-gen
- Constipation: 15-20% vs. 3-5%
- Urinary retention in elderly: 5-8% vs. under 1%
The Bigger Risk: Cognitive Decline and Dementia
The most alarming thing about anticholinergic drugs isn’t dry mouth or constipation. It’s what they do to your brain. Long-term use of first-generation antihistamines is linked to a 54% higher risk of dementia over seven years, according to a landmark study published in JAMA Internal Medicine. The more you take, and the longer you take it, the worse it gets. Each extra year of use beyond 90 daily doses increases risk by 20%. The American Geriatrics Society calls these drugs “potentially inappropriate” for older adults. Their Beers Criteria-used by doctors nationwide-explicitly lists diphenhydramine and chlorpheniramine as drugs to avoid in people over 65. The European Academy of Allergy and Clinical Immunology goes even further: they say to avoid them entirely in seniors. One 72-year-old woman from Ohio told Consumer Reports, “I used Benadryl for 20 years. I didn’t realize how much my dry mouth and trouble peeing were part of my life until they vanished after switching to loratadine.”Who Should Avoid These Meds?
You should avoid first-generation antihistamines if you:- Are over 65
- Have an enlarged prostate
- Have constipation or bowel disorders
- Have glaucoma
- Have kidney or liver disease
- Take other anticholinergic drugs (like some antidepressants, bladder meds, or sleep aids)

What to Do Instead
Switching to a second-generation antihistamine is the easiest fix. Cetirizine, loratadine, fexofenadine, and levocetirizine are all available over the counter. They work just as well for allergies, with far fewer side effects. If you need help sleeping, try melatonin or a non-anticholinergic sleep aid. For cold symptoms, use saline sprays, humidifiers, and pain relievers instead of multi-symptom formulas that hide diphenhydramine. Check your medicine labels. Many cold and flu products list “PM” or “nighttime” formulas-those almost always contain diphenhydramine or doxylamine. Look for “non-drowsy” versions instead.When You Can’t Avoid Them
Sometimes, you have no choice. Maybe your doctor prescribed diphenhydramine for severe itching or motion sickness. If you must take it:- Start with half the dose (12.5 mg instead of 25 mg)
- Wait 72 hours before increasing it
- Drink plenty of water
- Chew sugar-free gum
- Take a daily fiber supplement or stool softener
- Monitor for urinary retention-especially if you’re male and over 50
The Future Is Changing
Hospitals are dropping first-generation antihistamines from their formularies. Mayo Clinic eliminated diphenhydramine entirely in 2022 because of delirium cases in older patients. The FDA added dementia warnings to labels in 2021. The European Medicines Agency banned them for kids under two. Newer drugs are coming. Olopatadine nasal spray (Patanase), approved in 2023, shows zero anticholinergic activity. Researchers are even testing H4 receptor blockers that target allergies without touching acetylcholine at all. But until then, the choice is yours. You don’t need to suffer dry mouth, constipation, or urinary problems just to manage allergies. There are better options. And if you’ve been taking these meds for years, it’s not too late to switch.Ask your pharmacist or doctor to review your medications. You might be surprised how much better you feel without the hidden side effects.


12 Comments
I used to take Benadryl every night just to sleep. Didn’t think twice about it until my dentist started asking why my teeth were crumbling. Switched to Zyrtec last year and my mouth doesn’t feel like a desert anymore. Also, no more midnight bathroom battles. Life changed.
The data presented here is statistically significant, yet the author commits a fundamental fallacy by conflating correlation with causation regarding dementia risk. The JAMA study adjusted for confounders inadequately-polypharmacy, socioeconomic status, and baseline cognitive decline were not fully controlled. This is pseudoscience dressed in peer-reviewed clothing.
Bro. I just found out my ‘sleep aid’ was basically a brain fog pill. 😳 I’ve been taking that $5 bottle of diphenhydramine since college. My wife says I’ve been ‘off’ for years. Guess I’m switching to Claritin now. Also, why does every cold medicine have this crap in it? Like, who thought this was a good idea??
I never realized how much my dry mouth and constipation were tied to my allergy meds until I stopped them. I thought it was just aging. Turns out, it was the Benadryl. My GI doc was shocked I’d been taking it for 12 years. Now I use a neti pot and loratadine. So much better. Why isn’t this common knowledge?
Y’all need to stop the panic 😅 I get it, dry mouth sucks. But don’t throw the baby out with the bathwater. If you’re young and healthy and only use it once in a while for a bad allergy day? Chill. It’s not gonna turn you into a dementia patient tomorrow. Just don’t make it your nightly ritual. 🙏
So we’re supposed to pay $18 for a pill that works the same as the $4 one? Brilliant. The real anticholinergic effect here is on my wallet. Thanks, Big Pharma, for making me choose between my bladder and my bank account.
I switched to Allegra last month and I feel like a new person!! My energy is back, I’m not constipated anymore, and I can actually pee without feeling like I’m trying to start a car in winter 🙌 I didn’t even know I was suffering until it was gone. Thank you for this post!!
This isn’t just about medication-it’s about how we’ve normalized pharmacological compromise in daily life. We accept cognitive fog, constipation, urinary dysfunction as ‘normal side effects’ because we’ve forgotten what it feels like to be fully present in our own bodies. The real tragedy isn’t the drug-it’s the cultural acceptance of diminished function as inevitable.
They say anticholinergics cause dementia but what they dont tell you is the FDA and pharma are hiding the real cause-5G brain waves. Diphenhydramine is just a distraction. Look at the patent filings. The real goal is to make people dependent on expensive meds so they dont notice the mind control. I used to take it daily. Now I drink apple cider vinegar and sleep in a tin foil hat. Fixed.
Why do people even care? It’s just dry mouth. You drink water. Constipation? Take a laxative. Urinary issues? Catheter. Dementia? So what? People die anyway. Stop being dramatic. The real problem is you’re too lazy to just deal with it.
OMG I’m telling my mom right now!! She’s been on Benadryl for 15 years for ‘allergies’ and ‘sleep’ and I swear she’s been so forgetful lately. I’m taking her to the pharmacist tomorrow. She’s 71 and I didn’t even connect the dots. Thank you for this. 💕 You just might’ve saved her brain 🤍
It’s amusing how the author presents this as some groundbreaking revelation. The anticholinergic burden index has been in clinical use since the early 2000s. The Beers Criteria were published in 1991. Anyone with a medical degree knows this. The real issue is laypeople consuming pharmaceutical marketing masquerading as healthcare advice. The solution isn’t switching antihistamines-it’s improving medical literacy.