Contact Dermatitis Type Checker
Determine Your Dermatitis Type
Answer these questions to help identify whether your contact dermatitis is more likely allergic or irritant. This tool is for informational purposes only and not a substitute for professional medical advice.
Your Results
Recommendations
Important: This tool provides general information only. It is not a substitute for professional medical diagnosis. If your symptoms persist or worsen, please consult a dermatologist.
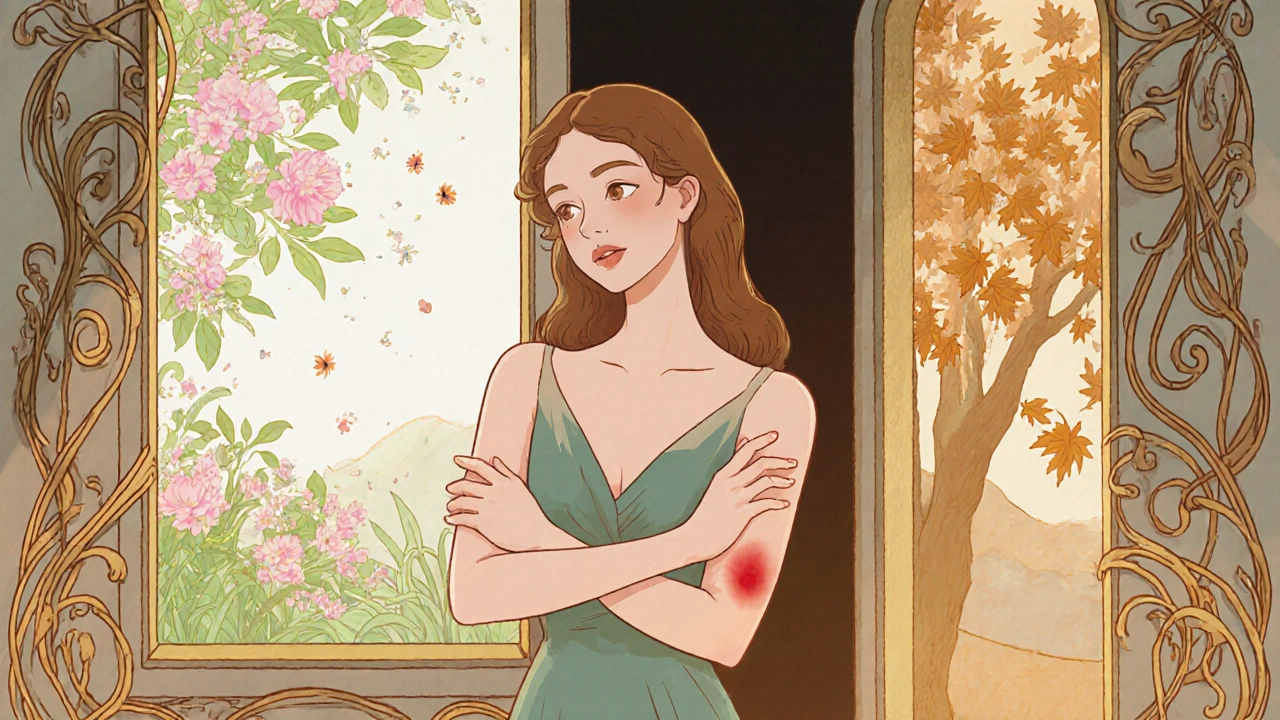
When the weather shifts, many people notice their skin reacting in ways that feel frustrating and uncomfortable. Contact dermatitis is a type of skin inflammation that occurs after direct exposure to an irritant or allergen. It shows up as redness, itching, swelling, and sometimes blisters. Understanding why seasonal changes trigger flare‑ups and what you can do about them is the first step toward lasting relief.
Key Takeaways
- Identify whether your dermatitis is allergic or irritant based on symptoms and exposure history.
- Adjust your skin‑care routine to match humidity and temperature swings.
- Use barrier protection (gloves, long sleeves) during high‑risk activities.
- Apply moisturizers and prescribed topical corticosteroids promptly during a flare.
- Seek professional help if symptoms persist more than two weeks or spread rapidly.
1. Why Seasonal Shifts Matter
Spring brings pollen and higher humidity, while autumn drops temperatures and dries out indoor air. These changes affect the stratum corneum-the outer layer that keeps moisture in and irritants out. When humidity falls, the skin loses water faster, cracking the barrier and letting irritants slip through. Conversely, a humid day can amplify the spread of allergens like plant oils or mold spores.
Two main forms of Allergic contact dermatitis occurs when the immune system reacts to a specific chemical or protein, triggering an allergic response that can linger for weeks and Irritant contact dermatitis results from direct damage to the skin by substances such as soaps, detergents, or extreme temperatures, often appearing quickly after exposure respond differently to seasonal triggers. Knowing which type you have helps you target the right prevention tactics.
2. Pinpointing Your Triggers
Start a simple diary: note the date, weather, what you wore, any products you used, and how your skin felt. After a couple of weeks you’ll see patterns-perhaps a rash after gardening in spring or after using a new laundry detergent in autumn.
For a definitive answer, Patch testing is a procedure performed by a dermatologist where small amounts of suspected allergens are applied to the skin under adhesive patches to observe reactions over 48‑96 hours is the gold standard. The test can differentiate allergic from irritant reactions and identify specific culprits like nickel, fragrance mixes, or topical antibiotics.
While waiting for test results, eliminate obvious offenders: avoid scented lotions, switch to fragrance‑free laundry soap, wear cotton gloves when handling cleaning products, and rinse new clothes before wearing them.
3. Building a Seasonal Skin‑Care Routine
Moisturizing is the backbone of any dermatitis plan. Choose a product that restores lipids and seals in water. Look for ingredients such as ceramides, hyaluronic acid, and petrolatum. Apply moisturizer within three minutes of showering while the skin is still damp; this locks in up to 80% more moisture.
During dry winter months, increase the frequency to two or three times daily. In humid summer, a lighter, non‑comedogenic lotion may feel more comfortable, but never skip the protective layer.
Consider adding a Humidifier an appliance that adds moisture to indoor air, helping to prevent skin drying caused by heating systems in bedrooms and living areas during the colder season. Aim for indoor humidity around 45‑55% for optimal skin barrier function.

4. Protecting Your Skin Outdoors
When temperatures rise or pollen counts spike, your skin faces a double assault: UV radiation and airborne allergens. Shielding your skin reduces both irritation and the risk of sun‑burn, which can worsen dermatitis.
- Clothing: Wear long sleeves made of breathable fabrics like linen or tightly‑woven cotton. For gardening, use nitrile gloves that don’t have the latex proteins many people react to.
- Sunscreen: Choose a mineral sunscreen (zinc oxide or titanium dioxide) without fragrance. Apply at least 15 minutes before heading out and reapply every two hours.
- Barrier creams: Before handling potential irritants (e.g., lawn fertilizers), apply a thick barrier cream containing dimethicone to create a protective film.
5. Managing an Acute Flare‑Up
When a rash erupts, act quickly to stop the cycle of itching and inflammation.
- Cool compress: Apply a clean, cool (not icy) cloth for 10‑15 minutes to soothe heat and reduce swelling.
- Cleansing: Use a mild, fragrance‑free cleanser. Avoid hot water; lukewarm is best.
- Medication: Over‑the‑counter hydrocortisone 1% can calm mild inflammation. For moderate to severe cases, a Topical corticosteroid prescription‑strength creams such as betamethasone or clobetasol that reduce immune activity in the skin, prescribed by a dermatologist may be necessary.
- Moisturize: Apply a thick ointment (e.g., petrolatum‑based) immediately after the steroid to lock in moisture and minimize steroid‑induced skin thinning.
- Antihistamine: An oral, non‑sedating antihistamine (like cetirizine) can curb itching, especially if an allergic component is suspected.
Never scratch-scratching breaks the skin barrier further and can introduce infection. Keep fingernails trimmed short, and consider wearing soft cotton gloves at night if itching intensifies.
6. When to See a Professional
If your rash spreads beyond the original contact site, shows pus or crusty ooze, or fails to improve after two weeks of home care, book an appointment with a Dermatologist a medical doctor specialized in skin, hair, and nail disorders, capable of prescribing stronger treatments and performing diagnostic tests. They may recommend systemic treatments such as oral steroids, immunosuppressants, or phototherapy for chronic cases.
Special attention is needed for children, pregnant women, or people with existing conditions like asthma or eczema, as they may react differently to medications.

7. Long‑Term Strategies for Year‑Round Comfort
Beyond the immediate tactics, adopt habits that keep your skin resilient throughout the year.
- Diet: Incorporate omega‑3 fatty acids (found in fish, flaxseed, walnuts) which support skin barrier health.
- Stress management: High stress can flare dermatitis. Practices such as mindfulness, yoga, or simple breathing exercises have been shown to reduce itch intensity.
- Regular check‑ins: Review your skin diary each season and adjust products accordingly. What worked last spring may need tweaking this fall.
Comparison: Irritant vs. Allergic Contact Dermatitis
| Feature | Irritant Contact Dermatitis | Allergic Contact Dermatitis |
|---|---|---|
| Onset | Minutes to hours after exposure | 12‑72 hours after exposure |
| Cause | Direct skin damage (e.g., soaps, acids) | Immune‑mediated reaction to allergen |
| Typical Triggers | Detergents, solvents, extreme temperature | Nickel, fragrance mix, latex, topical antibiotics |
| Distribution | Localized to contact site | Can spread beyond contact area |
| Treatment Focus | Avoid irritant, barrier repair | Avoid allergen, anti‑inflammatory meds |
Frequently Asked Questions
Can I use regular lotion on contact dermatitis?
Only if the lotion is fragrance‑free, dye‑free, and contains barrier‑restoring ingredients like ceramides or petrolatum. Regular scented lotions often add irritants that worsen the rash.
Is it safe to apply a steroid cream for a week?
Short‑term use (up to 2 weeks) of low‑ to medium‑strength steroids is generally safe. Prolonged use without a doctor’s oversight can thin the skin and cause other side effects.
Do antihistamines help with contact dermatitis?
They can reduce itching, especially when an allergic component is present, but they don’t treat the underlying inflammation. Pair with topical therapy for best results.
How often should I replace my humidifier water?
Clean the tank daily and replace the water every 24‑48 hours to prevent mold growth, which could introduce new allergens.
Can diet affect contact dermatitis?
While diet isn’t a direct cause, foods rich in omega‑3 fatty acids and antioxidants support skin barrier health and may lessen flare severity.
Next Steps
Start by documenting your symptoms for a week. Replace your current cleanser with a mild, fragrance‑free alternative and add a thick moisturizer after each shower. If you notice a pattern linking a product or activity to a flare, eliminate it and consider scheduling a patch test with a dermatologist.
Remember, seasonal changes are inevitable, but with the right routine and a little foresight, you can keep Contact dermatitis under control year‑round.

8 Comments
Maintaining the integrity of the stratum corneum across seasonal transitions requires a concerted effort to synchronize environmental control, product selection, and behavioral habits, all of which collectively reinforce the skin’s natural barrier function; this synchronization is best achieved through meticulous documentation and proactive adjustments, rather than reactive measures after a flare has taken hold. By instituting a daily skin‑care log that records ambient humidity, temperature, and the specific moisturizers or cleansers applied, individuals can identify subtle correlations that might otherwise be obscured by the sheer volume of daily variables. In addition, employing a humidifier calibrated to maintain indoor relative humidity between 45 and 55 percent ensures that the epidermal water content remains stable, thereby minimizing transepidermal water loss that can predispose to irritant contact dermatitis. Selecting barrier repair moisturizers that contain ceramides, petrolatum, and hyaluronic acid, and applying them within three minutes of a lukewarm shower, creates a lipid‑rich film that seals in moisture while also providing a protective scaffold for compromised skin cells. It is advisable to alternate between a heavier ointment, such as a petrolatum‑based product, during the arid months and a lighter, non‑comedogenic lotion in the higher‑humidity periods, thereby preventing both excessive occlusion and insufficient hydration. For individuals who must engage in activities with known irritants, such as gardening or handling cleaning agents, the use of nitrile gloves-free of latex proteins-and pre‑application of a dimethicone‑based barrier cream can significantly attenuate the direct chemical assault on the epidermis. Moreover, periodic patch testing under the guidance of a dermatologist remains the gold standard for distinguishing allergic from irritant mechanisms, facilitating targeted avoidance strategies once specific allergens are identified. When an acute flare does occur, the immediate implementation of a cool compress for ten to fifteen minutes, followed by gentle cleansing with a fragrance‑free, pH‑balanced cleanser, can alleviate inflammation and prevent secondary infection. Topical corticosteroids of appropriate potency, prescribed after a professional evaluation, should be applied for the shortest effective duration to mitigate the risk of skin atrophy, and subsequently followed by a thick emollient to reinforce barrier recovery. Finally, incorporating dietary sources of omega‑3 fatty acids, such as cold‑water fish or flaxseed, supports the biochemical pathways involved in barrier lipid synthesis, further enhancing resilience against seasonal provocations. In sum, a systematic, data‑driven approach that combines environmental modulation, judicious product use, protective attire, and medical oversight offers the most robust defense against the cyclical challenges posed by contact dermatitis.
Honestly, most of this guide just rehashes the basics you can find on any dermatologist’s brochure, and the emphasis on moisturizers feels like a sales pitch for the lotion aisle.
Keeping a concise diary for a couple of weeks really helps to pinpoint weird triggers like a new laundry detergent or a change in fabric softener, and once you spot the pattern you can cut it out before it becomes a full‑blown flare.
Hey folks, don’t forget that staying hydrated internally is just as important as slathering on moisturizer-drink plenty of water and you’ll notice your skin feels more supple during those dry winter months.
What most people overlook is that many so‑called “natural” humidifiers actually disperse microscopic particles of mold and bacterial spores, which can act as hidden allergens that exacerbate both irritant and allergic contact dermatitis, especially when the device is not cleaned regularly; this hidden risk is compounded by the fact that manufacturers rarely disclose the exact composition of the emitted mist, leading to a covert exposure scenario that fuels chronic skin inflammation, and the only way to mitigate this is to use distilled water, clean the unit daily, and consider a UV‑sterilizing filter if you’re serious about protecting your skin from invisible invaders.
I appreciate the thoroughness of this guide and want to stress that if a flare persists beyond two weeks despite diligent home care, you should assertively schedule an appointment with a board‑certified dermatologist to explore prescription‑strength options and possibly undergo patch testing for elusive allergens.
the thing about skin is that it’s a reflection of your inner chaos so if you’re stressed your skin will scream you need to chill out and maybe try some meditation or just breathe deep
Utilizing a ceramide‑enriched barrier repair ointment yields quantifiable improvements in transepidermal water loss metrics.