You’re looking at a blank wall, or maybe the sky, and suddenly-there it is. A dark spot drifts across your vision. Then a flicker of light, like a spark behind your eyelid. You blink. It’s gone. Then it comes back. If this has happened to you, you’re not alone. Around 75% of people over 65 experience floaters and flashes at some point. Most of the time, they’re harmless. But sometimes, they’re a warning sign you can’t afford to ignore.
What Are Floaters and Flashes?
Floaters are those little specks, threads, or cobweb-like shapes that seem to drift when you move your eyes. They’re not on your eye’s surface-they’re inside, floating in the vitreous, the clear gel that fills the space between your lens and retina. As you age, this gel slowly breaks down. Collagen fibers clump together, casting shadows on your retina. That’s what you see. Flashes are different. They’re not objects. They’re lights. Brief streaks, sparks, or lightning-like bursts, usually at the edge of your vision. These happen when the shrinking vitreous tugs on the retina. Your retina doesn’t sense light from the outside-it senses pressure. So when it gets pulled, it sends a signal to your brain that looks like a flash of light. Both are symptoms, not diseases. But knowing the difference between normal aging and something serious can save your sight.Why Do They Happen? The Science Behind the Vitreous
Your eye’s vitreous is mostly water-99%-with a network of collagen fibers holding it together like a sponge. Around age 40, that sponge starts to dry out and shrink. This is called vitreous syneresis. By your 60s or 70s, it’s common for the vitreous to pull away from the retina entirely. This is called posterior vitreous detachment (PVD). It happens in about 66% of people over 70. When the vitreous detaches, it can tug on the retina. Sometimes, that tug is gentle. You get a few new floaters and maybe a few flashes. That’s usually PVD, and it’s normal. But sometimes, the pull is strong. If the vitreous is stuck tightly to a weak spot on the retina, it can tear the retina as it pulls away. That’s when things get dangerous. A retinal tear can lead to a retinal detachment-a sight-threatening emergency.How to Tell the Difference: Benign vs. Dangerous
Not all floaters and flashes are the same. Here’s how to tell if you’re dealing with a harmless change or something urgent:- Benign PVD: A sudden shower of a few new floaters, maybe one or two flashes over a day or two. Vision stays clear. No curtain or shadow. Symptoms fade over weeks or months as your brain learns to ignore them.
- Warning signs: A sudden burst of many new floaters (like a handful of black dots), persistent flashes (repeating every few seconds), a dark shadow creeping across your vision, or sudden blurry or lost peripheral vision. These are red flags.
Who’s at Higher Risk?
Some people are more likely to have complications:- People over 65: Risk of PVD climbs sharply after 65.
- Nearsighted individuals: Longer eyeballs mean more tension on the retina. PVD can hit them 10-15 years earlier.
- People with diabetes: High blood sugar can weaken retinal blood vessels. A bleed into the vitreous can mimic floaters but is far more serious.
- Those with eye trauma or surgery: Even old injuries can cause late-onset vitreous changes.
When to See a Doctor-Immediately
You don’t need to wait for symptoms to get worse. If you notice any of these, call your eye doctor or go to an emergency eye clinic the same day:- Sudden increase in floaters (especially if they look like a cloud or shower)
- Flashes that repeat over seconds or minutes
- A dark curtain or shadow moving across your vision
- Loss of side vision
- Sudden blurry vision that doesn’t clear up
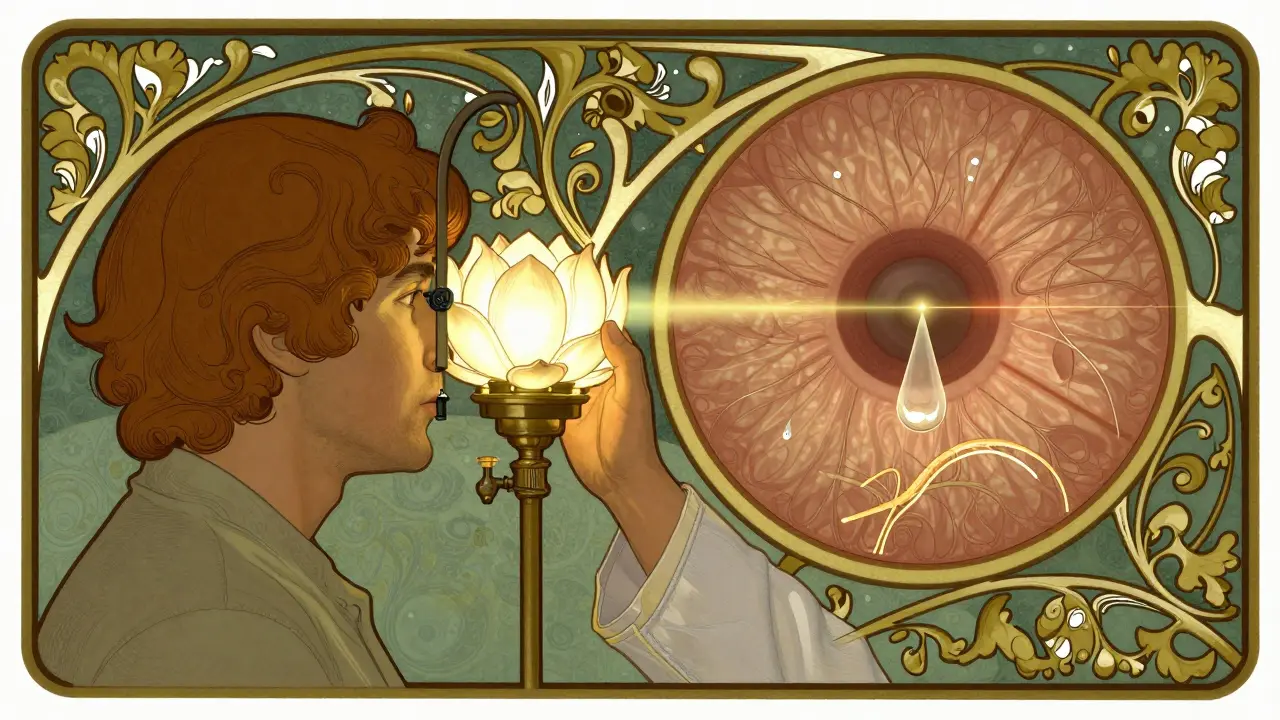
What Happens at the Eye Doctor?
Your eye care provider won’t just look at your eyes-they’ll dilate your pupils. That’s the only way to see the retina clearly. They’ll use a special lens to check for:- Retinal tears or holes
- Vitreous hemorrhage (blood in the gel)
- Signs of detachment
- Other conditions like inflammation or diabetic changes
Can Floaters Be Treated?
Most people don’t need treatment. Over six months, the brain adapts. The floaters settle lower in the eye, out of your central vision. They don’t disappear, but you stop noticing them. There are treatments-but they’re not for everyone.- Laser vitreolysis: A laser breaks up large floaters. It’s available in some clinics, but not widely covered by insurance. Results vary. It doesn’t work for everyone and carries a small risk of retinal damage.
- Vitrectomy: Surgery to remove the vitreous. Reserved for severe cases where floaters completely block vision. It’s invasive, carries risks like cataracts and infection, and is rarely recommended just for floaters.
What You Can Do Right Now
If you’ve just noticed floaters or flashes:- Don’t panic. Most cases are harmless.
- Don’t wait. Schedule an eye exam within 24-48 hours, even if symptoms seem mild.
- Write down what you’re seeing: How many floaters? When did they start? Are flashes happening repeatedly?
- Don’t drive if your vision is blurry or you have a shadow in your sight.
Final Thought: Your Eyes Are Unique
Floaters and flashes are common. But they’re not always normal. The difference between a harmless aging change and a sight-threatening emergency often comes down to timing and pattern. One doctor’s rule of thumb: If you’re unsure, get it checked. The good news? Most people who see a doctor get a clean bill of health. The better news? If something is wrong, catching it early means you can protect your vision with a simple, quick procedure. Don’t risk it. Book your eye exam. It takes less than an hour. Your sight is worth it.Are floaters and flashes always a sign of something serious?
No. Most floaters and flashes are caused by posterior vitreous detachment (PVD), a normal part of aging. Around 75% of people over 65 experience them. They’re usually harmless and become less noticeable over time. But sudden changes-like a burst of new floaters or repeated flashes-can signal a retinal tear or detachment, which requires urgent care.
How long do floaters last?
Floaters from PVD typically settle within six months. Your brain learns to ignore them, and the debris drifts out of your central vision. Some people notice them for a year or longer, but they rarely get worse. If floaters suddenly increase in number or change in appearance after months of stability, see your eye doctor.
Can stress or screen time cause floaters?
No. Stress and screen time don’t cause floaters. They can make you more aware of them-especially if you’re tired or staring at a bright screen-but they don’t create the physical changes in the vitreous that cause floaters. The real cause is aging-related changes inside the eye.
Should I be worried if I only have flashes and no floaters?
Yes. Flashes alone can still mean the vitreous is pulling on the retina. Even without new floaters, repeated flashes-especially if they happen in clusters-can indicate a retinal tear. You should still get examined within 24-48 hours. Don’t wait for floaters to appear.
Is it safe to wait a few days to see a doctor?
If you have sudden, numerous floaters or repeated flashes, no. You should be seen the same day. Retinal tears can progress to detachment within hours. If symptoms are mild and stable-like a few floaters and one or two flashes over a day-it’s usually safe to wait 24-48 hours for a routine appointment. But if symptoms worsen at any point, go immediately.
Can floaters come back after treatment?
If you’ve had a retinal tear treated with laser, the tear won’t come back. But new floaters can still form as the vitreous continues to age. Laser vitreolysis can reduce existing floaters, but it doesn’t stop new ones from forming. Vitrectomy removes the vitreous, but it’s rarely done just for floaters due to risks. Most people learn to live with them.


12 Comments
Just had my annual eye exam last week - no floaters yet, but I’m already paranoid 😅 Thanks for the clear breakdown! I’m booking my next one in 6 months, no excuses.
Bro, I’m 42 and got flashes last month. Thought it was just my phone screen. Turned out it was PVD. Doc said I’m lucky it wasn’t a tear. Don’t ignore it - even if you’re young. India’s got tons of people skipping eye checks. Don’t be one.
I used to think floaters were just stress. Turns out they’re just my eyeballs aging like a fine wine. Kinda weird to think about, but also kind of beautiful? Anyway, got my appointment booked. Thanks for the nudge.
Typical American overreaction. In Britain, we wait until we’re blind before seeing a doctor. Saves time. And money. And unnecessary anxiety.
THIS IS WHY AMERICA IS FALLING APART!!! PEOPLE IGNORE SYMPTOMS BECAUSE THEY’RE TOO LAZY TO DRIVE TO AN OPTOMETRIST!!! YOU THINK YOUR PHONE SCREEN CAUSES RETINAL TEARS??? GET A CLUE!!!
My uncle in Delhi had this. He waited. Lost half his vision. Now he’s blind in one eye. Don’t be like him. You think you’re invincible? You’re not.
Just had a vitreous detachment last year - 48, nearsighted. Flashes were wild. Got laser sealed in 20 mins. No downtime. Seriously, if you’re over 40 and see sparkles? Go. Don’t wait. Your retina doesn’t care about your schedule.
My grandma’s 84 and still sees floaters every day. She says they’re like little ghosts dancing in her vision. She’s got the best attitude about it. Just learned to live with them. Kinda beautiful, really.
The science here is impeccable. The vitreous’s collagen network undergoes syneresis due to age-related dehydration, leading to shadowing on the retinal photoreceptors. The mechanical traction on the retina generates phosphenes - not true visual stimuli, but neurologically interpreted as light. This is not anecdotal; it’s biomechanical physiology. Please consult a board-certified ophthalmologist if symptoms are acute.
Thank you for this comprehensive, evidence-based overview. The distinction between benign PVD and retinal pathology is critical, and this article clarifies it with precision. The emphasis on timing and pattern - rather than isolated symptoms - is clinically sound and should be widely disseminated.
I’ve had floaters since I was 30. They’re annoying but I don’t panic. I just move my eyes fast - they drift away. Still got my yearly checkups. Your eyes are your only pair. Treat ‘em right.
Just wanted to say - if you’re reading this and you’re scared? You’re not alone. I was terrified too. But I went in. Turned out fine. You’re doing the right thing by even looking this up. That’s courage.