When you need extra oxygen at home, it’s not just about plugging in a machine. It’s about staying alive, staying safe, and still being able to live your life-whether that means walking to the mailbox, watching TV, or hugging your grandkids. But here’s the hard truth: home oxygen therapy saves lives, but it also kills if you don’t treat it with serious respect. Fire doesn’t need much to turn deadly when oxygen is in the room. One spark, one slip-up, and everything changes. This isn’t scare tactics-it’s science. And it’s real.
Why Oxygen Is Dangerous (Even Though It’s Not Flammable)
Oxygen itself doesn’t catch fire. But it makes everything else burn faster. Like a jet engine for your couch, your blanket, your hair, even your clothes. Normal air is 21% oxygen. When you’re on therapy, the air around you can hit 40%, 50%, even 60% oxygen. That’s not just a little boost-it’s a fuel multiplier. A cigarette that normally smolders for 10 seconds can ignite in under one. A static shock from your synthetic blanket? Gone in a flash. A hair dryer left too close? Boom. The Oxygen concentrator is a device that pulls oxygen from room air and delivers it through tubing. It’s quiet, reliable, and runs on electricity. But if it’s blocked, overheated, or near a heat source, it’s not just useless-it’s a hazard.
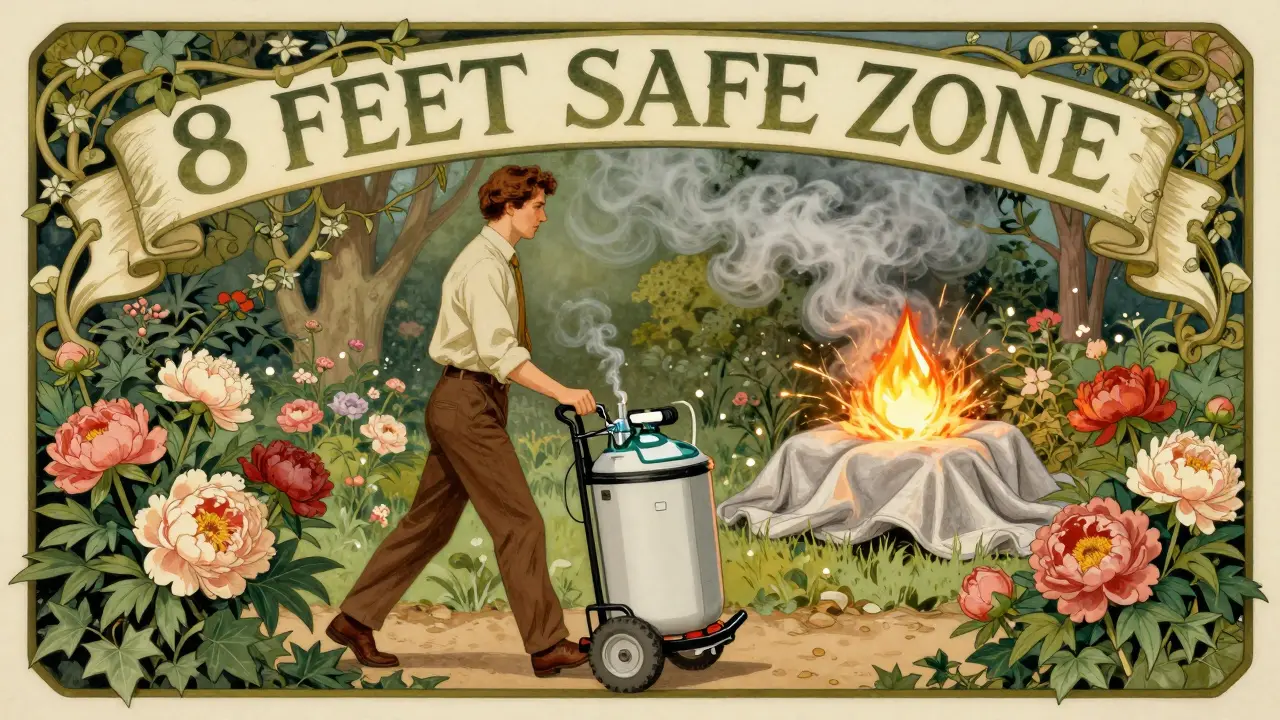
The numbers don’t lie. Between 2014 and 2018, U.S. fire departments responded to nearly 2,500 home fires involving oxygen equipment every year. Fifteen people died. Over 100 were injured. Twelve million dollars in property damage. Most of these fires? Started within 5 feet of the equipment. The National Fire Protection Association (NFPA) is a standards organization that sets fire safety codes now says 8 feet is the minimum safe distance. Not 5. Not 6. 8 feet. That’s from your heater, your lamp, your stove, even your toaster.
Three Types of Oxygen Systems-and Their Risks
Not all oxygen systems are the same. And each has its own danger zone.
- Oxygen concentrators are electric devices that filter air to deliver medical-grade oxygen. They’re the most common. No tanks to refill. Just plug them in. But they need space-6 inches from walls, 8 feet from heat. They also need clean filters. If you skip cleaning them every 2-4 weeks, the machine works harder, overheats, and can shut down. And if the power goes out? You’re out of oxygen unless you have a backup battery. Medicare requires 30 minutes of battery life, but many users don’t even know theirs is there.
- Compressed gas cylinders are metal tanks filled with oxygen under high pressure. They’re portable, but dangerous if dropped or exposed to heat. A damaged valve can turn the tank into a rocket-flying at 150 mph. These cause 68% of oxygen fires. Don’t store them in hot garages. Don’t leave them in cars. And never, ever try to refill them yourself.
- Liquid oxygen systems are cryogenic containers that store oxygen as a super-cold liquid. They hold more than tanks and last longer. But if they leak? The liquid hits -297°F. Skin contact causes instant frostbite. Spills can freeze carpets, floors, even your shoes. They’re heavy-15 to 30 pounds for the portable version-and increase fall risk for older users.
Most people start with concentrators. They’re safer, quieter, and don’t need refills. But if you’re out a lot, you’ll need a portable tank or liquid system. The key? Know which one you have-and what it can do to you if you’re careless.
The 10-Foot Rule: What You Must Do Every Day
Forget what you heard. The old 5-foot rule is outdated. New research from the American Thoracic Society is a professional organization that sets clinical guidelines for respiratory care shows flames spread 3.7 times faster in oxygen-rich air. So here’s what you need to do:
- Keep all flames-candles, lighters, stoves, grills-at least 10 feet away from your oxygen equipment. No exceptions.
- No smoking. Not even outside the door. Not even if you think the wind will carry it away. Oxygen lingers. It pools. It can ignite from across the room.
- Don’t use electric blankets, heating pads, or space heaters within 8 feet. Even if they’re "low heat," they create sparks.
- Keep hair dryers, electric razors, and power tools away. They generate sparks and heat. One 2022 FDA report found 18% of fires came from hair dryers alone.
- Use only cotton bedding and clothing. Synthetic fabrics build up static electricity. You won’t feel the shock-but oxygen will ignite it at 1,000 volts. You need 3,500 volts to feel it. That’s how sneaky this is.
- Never use oil-based lotions, creams, or petroleum jelly on your face or nose. They’re flammable. Use water-based products only.
- Keep oxygen tubing away from pets. Dogs and cats love to chew. A chewed tube leaks oxygen-and creates a silent hazard.
And if you have kids or visitors? Tell them. Put up signs. Use the American Lung Association’s Oxygen Safety Kit is a free resource with flame-resistant blankets and 10-foot zone markers. It’s simple. It works. And 83% of users say it made them feel safer.
Staying Active Without Risking Your Life
You don’t have to sit still. You can still walk. You can still shower. You can still go to church or visit family. But you need to plan.
Portable oxygen is key. If your concentrator is stationary, get a portable oxygen concentrator is a battery-powered device that delivers oxygen on the go. Most last 4-8 hours on a charge. Some go longer. Always carry a spare battery. And never leave it charging in your car-it can overheat.
For mobility: Use a wheeled cart for your concentrator. Don’t drag tubing across the floor. Tripping is the #1 cause of falls among oxygen users. Install ceiling-mounted tubing systems. They’re pricey, but Mayo Clinic data shows they cut falls by 43%. Or use Velcro straps to keep tubing pinned to walls or furniture. It’s cheap. It’s easy. And it saves lives.
Showering? No problem. Use a nasal cannula (the little tubes in your nose) instead of a mask. Masks can fog up. Cannulas let you breathe normally. Just keep the concentrator outside the bathroom. Water and electricity don’t mix. And don’t use a humidifier unless your doctor says so. Too much moisture can damage the machine.
Traveling? Call your oxygen provider ahead of time. Airlines require 48 hours’ notice. Make sure your device is FAA-approved. And always bring extra batteries-twice as many as you think you’ll need.
What Happens When Something Goes Wrong?
Most people think: "If I smell smoke, I’ll call 911." But you don’t have time to wait. Oxygen fires spread faster than you can react.
Here’s your emergency plan:
- If you see flames, turn off the oxygen source immediately. Unplug the concentrator. Close the valve on the tank.
- Get out. Don’t try to put out the fire. Don’t grab a towel. Just leave.
- Call 911 from outside. Don’t use your phone inside-it can spark.
- If you can’t turn off the oxygen, leave the house and shut the door behind you. That slows the fire.
- Never use water on an oxygen fire. It can make it worse.
Practice this once a month. With your caregiver. With your spouse. With a neighbor. Make it automatic. Because when panic hits, you won’t remember what to do.
Training Isn’t Optional-It’s Required
You wouldn’t drive a car without a license. But too many people get oxygen without training. The Centers for Medicare & Medicaid Services (CMS) is the U.S. government agency that oversees health coverage programs requires providers to give 3-5 hours of safety training. But a 2022 survey found 67% of patients got little to none.
You need to know:
- How to clean your filters
- How to check for leaks (listen for hissing, feel for cold spots)
- How to replace tubing (every 2-4 weeks)
- How to recognize if your machine isn’t working (red lights, alarms, weak flow)
- How to use your backup battery
Ask for the American Association for Respiratory Care (AARC) is a professional group that sets clinical standards for respiratory care 20-minute online safety module. It’s free. It’s short. And if you complete it, you’re 68% less likely to make a safety mistake. Most providers won’t offer it unless you ask.
What’s Changing in 2026?
The rules are getting stricter-and smarter.
Starting in 2025, Medicare will require all new oxygen equipment to shut off automatically within half a second if it detects a flame. New concentrators like the Philips Respironics SimplyGo Mini+ is a smart oxygen device with AI-powered flame detection already do this. They can sense a fire 18 inches away-and cut the flow before you even smell smoke.
And in 2024, the American Lung Association launched a certification program for home oxygen providers called Oxygen Safety Ambassador. These providers are trained to teach safety, not just deliver equipment. If your provider has this badge? You’re in good hands.
But technology won’t save you if you ignore the basics. No AI replaces common sense. No alarm replaces awareness.
Final Word: Oxygen Is a Lifeline-Not a Luxury
You’re not being paranoid. You’re being smart. Every rule, every distance, every warning? It’s there because someone died because they didn’t know.
Use your oxygen. Live your life. Walk outside. Visit friends. Laugh. Cry. Breathe. But never forget: oxygen doesn’t care if you’re tired, if it’s cold, if you’ve been doing this for years. It only reacts. And when it reacts? It burns.
Stay safe. Stay informed. Stay alive.
Can I use an electric blanket with home oxygen therapy?
No. Electric blankets, heating pads, and space heaters create sparks and heat, both of which can ignite oxygen-enriched air. Even on low settings, they’re dangerous within 8 feet of oxygen equipment. Use cotton blankets instead, and keep all heat sources at least 10 feet away.
Is it safe to smoke if I’m on oxygen therapy?
Absolutely not. Smoking while on oxygen therapy is one of the leading causes of fatal fires. Oxygen makes flames spread 3.7 times faster. A cigarette that normally smolders can ignite in under a second. Even smoking outside the house is risky-oxygen can linger in the air and be drawn back inside. Never smoke anywhere near oxygen equipment.
How often should I clean my oxygen concentrator filter?
Clean the filter every 2 to 4 weeks, depending on dust levels in your home. If you have pets, live near a road, or have construction nearby, clean it weekly. A clogged filter makes the machine work harder, reduces oxygen output, and can cause overheating. Always use the filter recommended by the manufacturer.
What should I do if my oxygen concentrator stops working?
First, check the power cord and outlet. Try a different outlet. If it still doesn’t work, switch to your backup oxygen source-whether that’s a portable tank or liquid system. If you don’t have a backup, call your oxygen provider immediately. Never try to fix the machine yourself. If you’re having trouble breathing, call 911.
Can I travel with home oxygen therapy?
Yes, but you must plan ahead. Contact your oxygen provider at least 2 weeks before travel. They’ll help you get FAA-approved portable equipment and extra batteries. Airlines require 48 hours’ notice. Never check oxygen equipment as luggage. Carry it with you. Always bring twice as many batteries as you think you’ll need. And never use oxygen near open flames, including campfires or grills.
Do I need to use 100% cotton bedding?
Yes. Synthetic fabrics like polyester or nylon build up static electricity. You won’t feel a shock at 1,000 volts-but oxygen can ignite at that level. Cotton doesn’t build up static. It’s the safest choice for sheets, pajamas, and blankets. If you’re unsure, test a fabric by rubbing it with a balloon-if it sticks, it’s synthetic. Avoid it.
What’s the difference between a nasal cannula and an oxygen mask?
A nasal cannula delivers oxygen through two small tubes in your nostrils. It’s lightweight, quiet, and lets you talk, eat, and drink. An oxygen mask covers your nose and mouth and delivers higher flow rates, but can feel claustrophobic and fog up. Most people on home therapy use a cannula. Masks are usually for short-term use or higher oxygen needs.
Can I use petroleum jelly on my lips while on oxygen?
No. Petroleum-based products like Vaseline are flammable. Oxygen can cause them to ignite. Use water-based lip balms or moisturizers instead. Look for labels that say "oil-free" or "water-based." If you’re unsure, ask your oxygen provider or pharmacist.
How do I know if my oxygen equipment is Medicare-approved?
Your oxygen provider must be Medicare-certified and supply equipment that meets UL 867 and UL 448 safety standards. Ask them for proof of certification. If they can’t show it, they’re not compliant. Non-certified devices make up 14% of the market-and they’re not safe. Always choose providers with a good reputation and clear safety training.
What should I do if I smell burning near my oxygen equipment?
Turn off the oxygen source immediately. Unplug the concentrator or close the tank valve. Get out of the house. Call 911 from outside. Do not try to put out the fire. Oxygen fires spread too fast. Your safety is more important than any equipment.


8 Comments
man i just got my oxygen concentrator last month and honestly i didnt realize how many things were dangerous around it. like i used to keep my electric blanket on low while i watched tv. now im using cotton sheets and keeping everything 10 feet away. weird how you dont think about static electricity until it could kill you lol
ok but why is everyone acting like oxygen is some kind of bomb?? i mean yeah it helps fire but so does alcohol and gasoline and we dont ban those. this whole 10ft rule feels like overkill. also why are we scared of hair dryers?? i use mine every day and nothing’s happened. maybe the real problem is people who dont know how to use basic appliances?? 😅
yo this post is life-saving. seriously. i lost my uncle last year because he thought "just one cigarette outside" was fine. oxygen lingers like ghost smoke. i got my portable concentrator now and i carry two batteries everywhere. also switched to water-based lip balm-no more Vaseline. small changes, big difference. stay safe out there 🙌
so we're now treating oxygen like it's a dragon in a cave? "beware the breath of life!" 🐉 the science is solid. but the tone here feels like a PSA from 1998. we're not in a fire drill. we're living. and yes, i still use my electric blanket. just not near the tubing. chill out. 😎
why does this article assume everyone has a caregiver, a backup battery, and a spare concentrator? what about people on fixed incomes? i can't afford a ceiling-mounted system or a $2000 portable unit. this isn't safety advice-it's privilege porn. "just buy more stuff" isn't a solution.
the 8ft rule changed to 10ft and now we're supposed to just accept it? i get the science but where's the real data on how many fires happened because someone was at 9ft? also i use a humidifier and my machine still works fine. maybe some of these rules need tweaking instead of just repeating them like gospel
Thank you for sharing this comprehensive and well-researched overview. The statistical references to NFPA, CMS, and FDA reports lend significant credibility to the safety guidelines presented. I would encourage all patients to request formal training from their providers, as many are unaware of the mandatory 3–5 hour requirement under Medicare regulations. Proactive education is the most effective prevention strategy.
you people are overthinking this. i’ve been on oxygen for 7 years. i smoke outside. i use my hairdryer. i sleep with a blanket. nothing’s happened. if you’re scared of your own oxygen machine, maybe you shouldn’t be using it. also… cotton sheets? really? my wife says i smell like a laundry commercial now 😂