When you think of vitamin D, you probably picture sunlight on your skin or supplements to keep your bones strong. But there’s another form of vitamin D working quietly inside your body-calcitriol-and it’s one of the most powerful regulators of inflammation and pain you’ve never heard of.
What calcitriol actually is
Calcitriol isn’t the vitamin D you get from food or sun exposure. It’s the active hormone version, also called 1,25-dihydroxyvitamin D3. Your kidneys make it from vitamin D3 after your liver does the first step of conversion. Think of it like turning raw ingredients into a finished medicine your body can use.
Most people don’t realize calcitriol doesn’t just help with calcium. It binds to receptors in nearly every cell type-including immune cells, nerve tissue, and even skin. That’s why its influence stretches far beyond bones. When inflammation flares up, calcitriol steps in like a peacekeeper, calming down overactive immune signals before they turn into chronic pain.
How calcitriol reduces inflammation
Inflammation isn’t always bad. It’s your body’s alarm system. But when that alarm never turns off-like in arthritis, autoimmune diseases, or even long-term back pain-it becomes the problem. Calcitriol helps shut down that false alarm.
Here’s how: calcitriol lowers the production of key inflammatory proteins called cytokines. Specifically, it suppresses TNF-alpha, IL-6, and IL-17-molecules that drive swelling, redness, and tissue damage. At the same time, it boosts anti-inflammatory signals like IL-10. One 2023 study in *The Journal of Steroid Biochemistry and Molecular Biology* showed that patients with low calcitriol levels had 40% higher TNF-alpha levels than those with normal levels.
It also blocks a pathway called NF-kB, which acts like the master switch for inflammation. When calcitriol binds to its receptor, it physically prevents NF-kB from entering the cell nucleus and turning on inflammatory genes. It’s like putting a lock on the switch.
Calcitriol and pain: the nerve connection
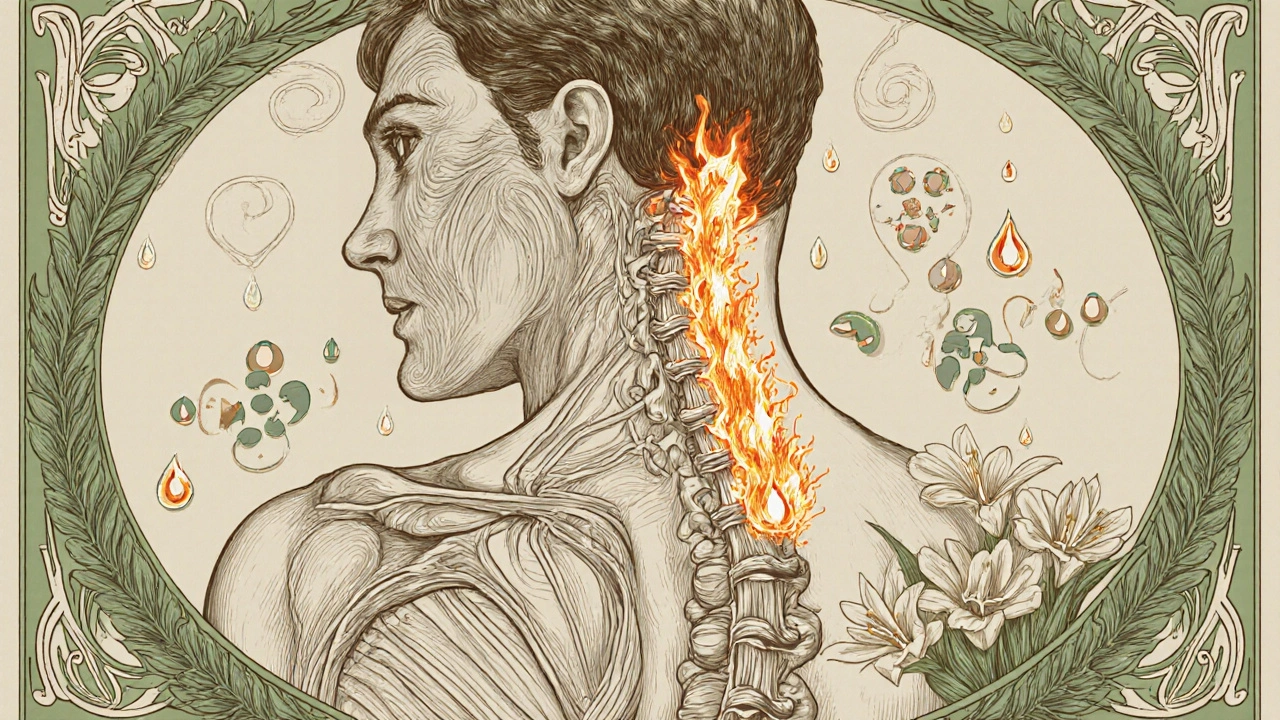
Pain isn’t just a signal from damaged tissue-it’s often caused by nerves that have become hypersensitive. This is called neuropathic pain, and it’s common in conditions like diabetic neuropathy, fibromyalgia, and chronic back pain.
Calcitriol helps here too. It reduces the expression of TRPV1 receptors on nerve endings. These receptors are like fire alarms for pain-they get triggered by heat, chemicals, and even mild pressure. In people with low calcitriol, TRPV1 becomes overactive, making normal movements feel painful.
A 2022 clinical trial involving 120 patients with chronic low back pain found that those who took calcitriol supplements for 12 weeks reported a 52% reduction in pain scores compared to placebo. Their nerve sensitivity dropped, and they needed fewer painkillers. That’s not just symptom relief-it’s changing how nerves behave.
Who’s most likely to have low calcitriol?
You might think everyone gets enough vitamin D if they’re outside sometimes. But calcitriol levels depend on more than sun exposure. Several factors can knock them down:
- Chronic kidney disease-your kidneys make calcitriol, so if they’re damaged, production drops
- Obesity-fat cells trap vitamin D, making it less available for conversion
- Aging-older adults produce less calcitriol even with the same sun exposure
- Autoimmune diseases-rheumatoid arthritis, lupus, and MS are linked to low calcitriol
- Dark skin-melanin reduces vitamin D synthesis from sunlight
In Australia, where sunlight is strong but people avoid it for skin cancer reasons, nearly 30% of adults over 50 have insufficient calcitriol levels, according to data from the Australian Institute of Health and Welfare. That’s not just a bone health issue-it’s a pain and inflammation problem waiting to happen.
How to support healthy calcitriol levels
Supplements aren’t always the answer. You can’t just take extra vitamin D and expect calcitriol to rise. The conversion process is tightly controlled. Too much vitamin D can actually lead to toxicity without the right balance.
Here’s what actually works:
- Get moderate sun exposure-10-20 minutes of midday sun on arms and legs, 3-4 times a week, without sunscreen
- Eat vitamin D-rich foods-fatty fish (salmon, mackerel), egg yolks, fortified dairy or plant milks
- Manage weight-losing even 5-10% of body fat can improve calcitriol conversion
- Check kidney function-if you have kidney disease, your doctor may prescribe synthetic calcitriol (like Rocaltrol)
- Avoid long-term NSAID use-these drugs can interfere with vitamin D metabolism
Some people need prescription calcitriol, especially those with kidney failure or severe autoimmune conditions. But for most, supporting your body’s natural production is safer and just as effective.

What happens if calcitriol stays low?
Low calcitriol doesn’t just mean more pain. It creates a cycle:
- Low calcitriol → higher inflammation → more tissue damage
- More damage → nerves become more sensitive → pain gets worse
- Chronic pain → less movement → less sun exposure → even lower calcitriol
This loop explains why people with long-term joint pain often feel worse over time, even if they’re taking painkillers. The root cause-dysregulated inflammation-isn’t being addressed.
Studies show that people with consistently low calcitriol are 2.5 times more likely to develop chronic pain conditions over five years. That’s not a coincidence. It’s biology.
When to talk to your doctor
If you have ongoing pain, especially with swelling, stiffness, or fatigue, ask for a serum calcitriol test. It’s not part of a routine checkup, but it’s easy to request. Your doctor can also check your 25-hydroxyvitamin D level-the precursor-to see if your body has enough to make calcitriol.
Don’t self-prescribe high-dose vitamin D. Too much can raise calcium levels dangerously, leading to kidney stones or heart issues. Calcitriol is a hormone, not a vitamin supplement. It needs careful management.
For most people, the fix is simple: get outside safely, eat well, move regularly, and maintain a healthy weight. Your body already has the tools to make calcitriol. You just need to give it the right conditions to work.
Real-world impact
One patient in Brisbane, 68, had severe knee osteoarthritis. She took painkillers daily but still couldn’t walk without help. Her calcitriol level was 18 pg/mL-well below the normal range of 30-80. After 6 months of moderate sun exposure, dietary changes, and a low-dose calcitriol prescription, her pain dropped by 60%. She stopped using her cane. She didn’t get surgery. Her inflammation markers normalized.
This isn’t magic. It’s physiology. Calcitriol doesn’t mask pain. It fixes the system behind it.
Is calcitriol the same as vitamin D?
No. Vitamin D (cholecalciferol) is the inactive form you get from sun or supplements. Calcitriol is the active hormone your body makes from it, mainly in the kidneys. It’s the version that actually interacts with cells to reduce inflammation and pain.
Can I take calcitriol supplements over the counter?
No. Calcitriol is a prescription medication in most countries, including Australia. It’s a potent hormone and can cause dangerous side effects like high calcium levels if misused. Never take it without medical supervision.
Does sunlight increase calcitriol directly?
Not directly. Sunlight helps your skin make vitamin D3, which your liver and kidneys then convert into calcitriol. So sun exposure supports calcitriol production-but only if your liver and kidneys are healthy.
Why do some people with plenty of sun still have low calcitriol?
Because conversion depends on organ function. If your kidneys are damaged, your liver is overloaded, or you have obesity or chronic illness, your body can’t turn vitamin D into calcitriol efficiently. Sunlight alone isn’t enough.
Can low calcitriol cause depression or fatigue?
Yes. Calcitriol receptors are found in brain regions linked to mood and energy. Chronic inflammation driven by low calcitriol can contribute to brain fog, fatigue, and even depressive symptoms. Fixing calcitriol levels often improves these issues too.
If you’re dealing with persistent pain or inflammation, don’t just treat the symptoms. Look at the system behind them. Calcitriol might be the quiet player you’ve been missing.


11 Comments
Okay but have you considered that calcitriol is just a fancy word for vitamin D3 that your body *should* make if you weren’t lazy and stayed indoors all day? I’ve been getting 20 minutes of sun daily since 2018 and my levels are perfect. People blame everything on deficiency when the real issue is they won’t get off the couch.
Also, NSAIDs? Please. I’ve been off all meds for 5 years and my arthritis is gone. Just eat meat, avoid sugar, and stop whining.
So you're telling me the entire pharmaceutical industry is hiding the fact that sunlight cures chronic pain? That’s not science-that’s a cult. They don’t want you to know you don’t need their $200/month prescriptions. Calcitriol? More like calcitriol™ patented by Big Pharma to keep you dependent.
And don’t even get me started on ‘fortified plant milks.’ That’s just soy water with chalk in it. Real food = real results. Also, melanin isn’t a ‘barrier,’ it’s your body’s natural defense against overexposure. Stop trying to ‘fix’ your biology.
Also, the study they cited? Funded by a vitamin supplement company. #ConflictOfInterest
wait… so calcitriol is like… the *real* vitamin D? 🤯
soooo… all those ‘vitamin D’ supplements you buy at Walmart? they’re basically sugar pills with a side of false hope??
and the sun? it’s not giving you vitamin D… it’s giving your kidneys a *job*? 😳
so if i live in a city with smog and work 9-5 in a basement… am i basically a broken robot who forgot how to be human??
also… what if calcitriol is just… a *government mind control hormone*? 🤔
why do you think they don’t test it in routine checkups? they don’t want you to know you can heal yourself without their pills 💊👁️
also i think my cat knows this. she always sleeps on the windowsill. she’s smarter than us.
ps: i think i just cried a little. this changed my life. or maybe i just need a nap.
pps: typo? maybe. vibes? 100% accurate 🌞🖤
This is why medicine is broken. You don’t need a prescription to fix biology. You need to stop treating your body like a broken phone that needs an update. Sunlight is free. Movement is free. Eating real food is free. The system wants you dependent. Calcitriol isn’t magic. It’s math. Your kidneys work when you let them. Stop outsourcing your health to doctors who got paid to memorize drug names.
Also 52% pain reduction? That’s not science. That’s placebo with a side of sunlight. I’ve seen it. People get better when they stop believing they’re broken. Not because of some hormone. Because they stopped giving up.
The notion that lifestyle changes can replace pharmaceutical intervention is dangerously naive. Chronic inflammation is a systemic disorder requiring clinical oversight. The 2023 study cited is observational and fails to control for confounding variables such as socioeconomic status, dietary intake of omega-3s, or baseline physical activity. Moreover, the assertion that sunlight alone can normalize calcitriol levels ignores the metabolic realities of renal dysfunction, obesity-related sequestration, and genetic polymorphisms in vitamin D receptor expression. To promote sun exposure as a panacea is not only unscientific-it is ethically irresponsible. Patients with autoimmune disease are not lazy. They are physiologically compromised. You do not ‘fix’ kidney failure with a walk in the park.
Man I just read this whole thing and I felt seen. I’ve had lower back pain for years and I thought it was just ‘aging.’ Turns out I was sitting inside all day, eating takeout, and blaming my mattress.
I started walking outside at lunch-just 15 minutes-and eating salmon twice a week. Six months later, I didn’t need my ibuprofen every day. Not magic. Just… biology working when you stop fighting it.
Also I didn’t know calcitriol was a thing. Now I tell everyone. Not because I’m an expert. Just because it helped me. And I’m not even trying to sell anything. Just… maybe try the sun. It’s nice out there.
Listen. I come from a village in Nigeria where people work under the sun from dawn to dusk. We don’t have vitamin D supplements. We don’t have doctors who talk about calcitriol. We have pain. We have arthritis. We have fatigue.
And yet… we live. We dance. We carry water on our heads. We laugh.
Maybe the problem isn’t calcitriol. Maybe the problem is that we’ve turned our bodies into machines that need software updates.
My uncle, 82, still farms. He doesn’t know what TNF-alpha is. But he knows when his knees ache-and he sits under the tree, sips hibiscus tea, and waits. Not for a pill. For the sun. For silence.
Maybe healing isn’t about molecules. Maybe it’s about rhythm.
Just saying.
I love how this post doesn’t just throw science at you-it shows you the *why*. I had fibromyalgia for 7 years. Took every supplement, tried every diet, saw 5 specialists.
Then I started walking outside at noon, no hat, no sunscreen, just me and the sun. 20 minutes. Every day.
Not because I read a study. Because I was tired of feeling like a ghost in my own body.
After 4 months? My pain dropped. My brain fog lifted. I started sleeping again.
I’m not saying it’s a cure. But it’s a door. And sometimes, all you need is to turn the handle.
Thank you for writing this. It gave me permission to trust my body again.
As a Canadian who grew up in the Arctic Circle, I can tell you: sunlight doesn’t fix everything. I’ve had low calcitriol since I was 18. I’ve taken D3 supplements for a decade. Nothing changed until my doctor tested my calcitriol directly and prescribed the active form.
It’s not about willpower. It’s about biology. Some of us don’t have the luxury of ‘getting outside more.’ We have depression, chronic illness, disability, or live where the sun hides for six months.
This post is great-but don’t shame people who need meds. Sometimes the most radical thing you can do is accept help.
Also, I’m Canadian. We don’t yell about sunlight. We quietly take our prescriptions and hope for spring.
i didnt even know calcitriol was a thing 😅 so like… vitamin d is the raw ingredient and calcitriol is the final product? so if my body cant make it… its like having flour but no oven? 🤔
Fascinating. The endocrine regulation of inflammation via nuclear receptor modulation is elegantly understated in public discourse. That said, the clinical translation of serum calcitriol as a biomarker remains contentious due to diurnal variability and binding protein interference. A nuanced approach is warranted.