Uric Acid & Immune System Risk Calculator
Enter your details below to assess your risk of immune-related complications from high uric acid levels.
Ever wondered why a simple blood test showing elevated uric acid can hint at more than just gout? When high uric acid hangs around, it doesn’t just settle in joints - it talks to your immune system, stoking inflammation and even nudging chronic disease risk. This guide unpacks the science, shows what it means for everyday health, and gives clear steps to keep both uric acid and immunity in check.
Quick Takeaways
- Hyperuricemia (uric acid >7mg/dL in men, >6mg/dL in women) triggers the NLRP3 inflammasome, a key driver of inflammation.
- Elevated uric acid amplifies neutrophil activity and cytokine release, weakening immune regulation.
- Long‑term high uric acid links to gout, kidney disease, cardiovascular issues, and higher autoimmune flare‑ups.
- Dietary tweaks (reduce purine‑rich foods, increase water intake) and medications (allopurinol, febuxostat) lower uric acid and calm immune over‑reaction.
- Monitoring uric acid alongside C‑reactive protein (CRP) and interleukin‑1β offers a fuller picture of inflammatory risk.
What Is Hyperuricemia?
Hyperuricemia is the medical term for consistently high levels of uric acid in the blood. Uric acid is a uric acid a waste product formed when the body breaks down purines, substances found in many foods and in DNA. Normally, kidneys filter and excrete most of it, keeping blood concentrations within a narrow range. When production outpaces excretion, or kidneys falter, levels rise.
The condition often flies under the radar because many people feel fine until a gout flare or kidney stone forces a doctor’s visit. Yet recent research shows that even modest elevations can silently prime immune cells, setting the stage for chronic inflammation.
How Uric Acid Talk to Your Immune System
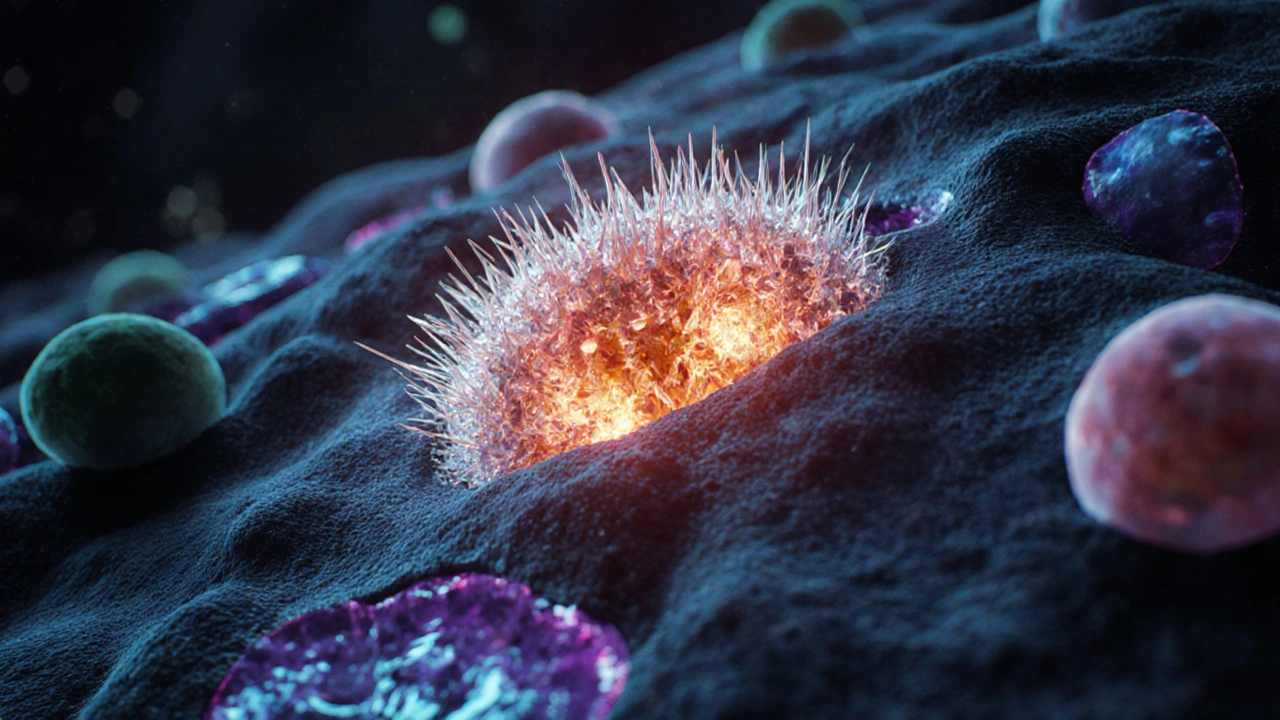
Uric acid isn’t just a passive by‑product; it can act as a danger‑associated molecular pattern (DAMP). When crystals form-especially monosodium urate (MSU) crystals-they are recognized by immune cells as a threat.
Key immune players include neutrophils the most abundant white blood cells, first responders that engulf pathogens and debris and cytokines signaling proteins like interleukin‑1β (IL‑1β) and tumor necrosis factor‑α (TNF‑α) that amplify inflammation. When MSU crystals lodge in tissues, neutrophils rush in, release reactive oxygen species (ROS), and die in a process called NETosis, spilling DNA traps that further irritate surrounding cells.
This cascade elevates oxidative stress an imbalance between free radicals and antioxidants, damaging proteins, lipids, and DNA, which feeds back into immune activation and can impair the body’s ability to combat infections.

The NLRP3 Inflammasome - The Central Switch
At the heart of uric‑acid‑driven inflammation sits the NLRP3 inflammasome a multi‑protein complex inside immune cells that, when activated, converts inactive pro‑IL‑1β into active IL‑1β. Crystal‑induced potassium efflux, lysosomal rupture, and ROS all converge on NLRP3, flipping the switch.
Once activated, NLRP3 releases mature IL‑1β and IL‑18, cytokines that recruit more immune cells, increase vascular permeability, and perpetuate pain and swelling. This mechanism explains why gout flares are so intense and why systemic inflammation can linger even after crystal clearance.
Clinical Consequences Beyond Gout
While gout is the most visible outcome, high uric acid’s impact reaches further:
- Kidney disease: Crystals can lodge in renal tubules, reducing filtration efficiency and encouraging hypertension.
- Cardiovascular risk: Epidemiological studies link hyperuricemia with higher rates of coronary artery disease, likely through endothelial dysfunction and chronic low‑grade inflammation.
- Autoimmune aggravation: Conditions like rheumatoid arthritis and systemic lupus erythematosus show worsened disease activity when uric acid spikes, possibly due to overlapping cytokine pathways.
- Metabolic syndrome: Elevated uric acid correlates with insulin resistance, obesity, and dyslipidemia, forming a vicious cycle with inflammation.
Clinicians now often monitor uric acid alongside CRP, ESR, and IL‑1β levels to gauge overall inflammatory burden.
Managing Uric Acid for a Healthier Immune Response
Good news: lifestyle and medication can tame both uric acid and the immune over‑reaction.
Dietary Strategies
- Limit purine‑rich foods: Red meat, organ meats, anchovies, and some legumes can boost uric acid production.
- Boost alkaline foods: Cherries, berries, and citrus have been shown in small trials to lower serum uric acid by up to 0.5mg/dL.
- Stay hydrated: Aim for at least 2.5L of water daily to help kidneys flush out uric acid.
- Moderate alcohol: Beer and spirits contain purines and impair renal excretion; occasional wine is less risky.
Pharmacological Options
| Drug | Mechanism | Typical Dose | Key Side Effects |
|---|---|---|---|
| Allopurinol xanthine oxidase inhibitor that blocks uric acid production | Inhibits xanthine → uric acid conversion | 100‑300mg daily | Rash, rarely Stevens‑Johnson syndrome |
| Febuxostat potent xanthine oxidase inhibitor, works even when allopurinol fails | Blocks xanthine oxidase more strongly | 40‑80mg daily | Elevated liver enzymes, cardiovascular alerts |
| Probenecid uricosuric agent that increases renal excretion of uric acid | Enhances renal tubular secretion | 250‑500mg twice daily | Kidney stones, gastrointestinal upset |
Targeting Inflammation Directly
When gout flares or systemic inflammation get out of hand, doctors may add colchicine, NSAIDs, or even IL‑1 blockers like anakinra. These agents blunt the downstream effects of NLRP3 activation, providing rapid symptom relief.
Monitoring Progress
Regular blood tests every 3‑6 months measuring:
- Serum uric acid
- CRP or ESR for general inflammation
- IL‑1β (if available) to gauge NLRP3 activity
Tracking these markers helps fine‑tune medication doses and lifestyle tweaks.
Checklist: Keep Uric Acid & Immunity in Balance
- Get a baseline uric acid test; aim for <7mg/dL (men) or <6mg/dL (women).
- Include a daily serving of cherries or berries.
- Drink 2‑3L of water; consider citrus‑flavored water if plain is boring.
- Limit red meat to twice a week; swap with fish low in purines like salmon.
- Schedule labs for uric acid, CRP, and kidney function every 4‑6 months.
- If on medication, review side effects with your doctor annually.
- Stay active - moderate exercise improves renal clearance and reduces insulin resistance.
Frequently Asked Questions
Can high uric acid cause infections?
Elevated uric acid itself doesn’t cause infections, but the chronic inflammation it generates can weaken immune regulation, making the body less efficient at fighting off pathogens.
Is gout the only symptom of hyperuricemia?
No. Many people have high uric acid without joint pain. They may develop kidney stones, hypertension, or subtle cardiovascular inflammation before any gout flare appears.
Do diet changes lower uric acid quickly?
Diet can lower levels by 0.3‑0.5mg/dL within a few weeks, especially when combined with increased water intake. For faster drops, medication is usually needed.
What is the role of the NLRP3 inflammasome in other diseases?
Beyond gout, NLRP3 drives inflammation in Alzheimer’s disease, type2 diabetes, and atherosclerosis. Targeting this pathway is an active area of drug research.
Can supplements like vitamin C help?
VitaminC modestly boosts renal excretion of uric acid, often dropping levels by 0.1‑0.2mg/dL. It’s a helpful adjunct but not a replacement for stronger interventions.

11 Comments
High uric acid really does more than just trigger gout; it can act as a danger‑associated molecular pattern that awakens the NLRP3 inflammasome, sending ripples through the immune landscape. By encouraging neutrophil recruitment and cytokine release, it creates a feedback loop that can magnify chronic inflammation. The good news is that lifestyle tweaks-like swapping out purine‑rich red meat for brighter plant‑based dishes-can blunt this cascade. Staying well‑hydrated, aiming for at least 2.5 L of water a day, helps the kidneys flush excess uric acid before crystals have a chance to form. If diet and hydration aren’t enough, medications such as allopurinol or febuxostat safely lower serum levels and give the immune system a breather. Regular check‑ups that track uric acid alongside CRP or IL‑1β give a clearer picture of where inflammation sits. Keep an eye on your numbers, and you’ll be steering your immune health in the right direction.
Staying on top of those labs can feel like a chore, but it’s really just a small step toward keeping your body balanced and feeling good.
Well,, you're telling us that drinking more water will magically erase uric acid's sneaky attacks??!! That's a bit of an oversimplification, isn't it? The whole purine‑rich diet thing is more complex than just saying 'eat less meat'-there are hidden sources everywhere, and many people can't just change theirs overnight. Also, the calculator seems to lump together male and female thresholds without acknowledging hormonal nuances. Just saying 'drink more' while ignoring kidney function? That's not a full picture.
Oh, please, you think a simple water‑intake tip solves the whole hyperuricemia saga? As if the body were a leaky bucket that you can just pour more liquid into and fix the crack! And don't get me started on the “just avoid red meat” advice-most folks can't just drop their favorite dishes without considering cultural and economic factors. Yet you present it with the same confidence as a textbook.
The pathophysiological nexus between hyperuricemia and immune dysregulation is anchored in the molecular detection of monosodium urate crystals by pattern‑recognition receptors, principally the NLRP3 inflammasome, which acts as a cytosolic electrochemical sentinel. Upon crystal engagement, potassium efflux, lysosomal destabilization, and mitochondrial reactive oxygen species converge to facilitate the assembly of the NLRP3‑ASC‑caspase‑1 complex. This proteolytic activation catalyzes the conversion of pro‑IL‑1β into its mature, bioactive form, setting off a downstream cascade that amplifies NF‑κB signaling and potentiates the secretion of TNF‑α, IL‑6, and IL‑18. The resultant cytokine milieu not only sustains local synovial inflammation characteristic of gout flares but also permeates systemic compartments, thereby influencing endothelial function and fostering a pro‑atherogenic phenotype. Concurrently, neutrophil extracellular trap (NET) formation, incited by crystal‑induced oxidative bursts, provides a scaffold for additional immune activation and perpetuates tissue injury. Importantly, the chronic low‑grade inflammation engendered by persistent uric acid elevation intersects with metabolic pathways, aggravating insulin resistance through interference with adiponectin signaling and perturbing hepatic gluconeogenesis. This metabolic‑immune crosstalk elucidates the observed epidemiological correlations between hyperuricemia and components of the metabolic syndrome, including hypertension, dyslipidemia, and obesity. Therapeutically, xanthine oxidase inhibitors such as allopurinol and febuxostat attenuate substrate availability, thereby reducing crystal burden and downstream inflammasome activation. However, emerging evidence suggests that adjunctive IL‑1 blockade (e.g., anakinra) may provide rapid amelioration of acute inflammatory spikes, especially in refractory cases. In practice, a multimodal approach that integrates dietary purine restriction, optimal hydration, and judicious pharmacotherapy yields the most robust attenuation of both uric acid load and inflammasome‑mediated immunopathology. Ongoing monitoring of serum uric acid alongside inflammatory biomarkers such as CRP and, where feasible, IL‑1β, enables dynamic risk stratification and therapeutic titration. Ultimately, the convergence of metabolic, renal, and immunologic factors necessitates a personalized management paradigm to mitigate the systemic sequelae of hyperuricemia.
Nice write‑up.
Ah, the tragic elegy of modern nutrition!-One is presented with a tableau of tables, charts, and bullet points, each promising salvation from the dreaded uric acid demon, yet the soul of the reader is left yearning for genuine clarity. Is it not a lamentable spectacle that we must wade through such labyrinthine jargon to discern a simple truth? Indeed, the veritable chorus of “reduce purines, drink water, avoid beer” sings in unison, but the opera of human physiology resounds far louder.
While the melodramatic prose is noted, the factual content suffers from grammatical inaccuracies: “drinks more water will magically erase” should read “drinks more water will magically erase” and “the whole purine‑rich diet thing” is too colloquial for a scientific discussion. Moreover, the statement that “allopurinol… safely lower serum levels” lacks a citation, which is essential for rigorous discourse.
People need to stop ignoring the moral side of this-if you keep eating steak and drinking beer while your kidneys suffer, you're basically choosing your own pain over community health.
Reflecting on the interplay between metabolic by‑products and immune vigilance invites us to view our bodies as holistic ecosystems rather than isolated systems. When uric acid accumulates, it sends a subtle alarm that can tip the balance toward inflammation, reminding us that diet, hydration, and even stress are threads woven into the same tapestry. By embracing a balanced plate-think colorful vegetables, modest portions of protein, and ample water-we nourish not just our muscles but also the silent guardians of our health. In this light, managing uric acid becomes a practice of stewardship, fostering resilience against both gout and broader inflammatory challenges.
Thank you for framing the issue so thoughtfully; adopting a holistic perspective indeed empowers individuals to make sustainable choices that benefit the immune system and overall wellbeing.