What Is Interstitial Lung Disease?
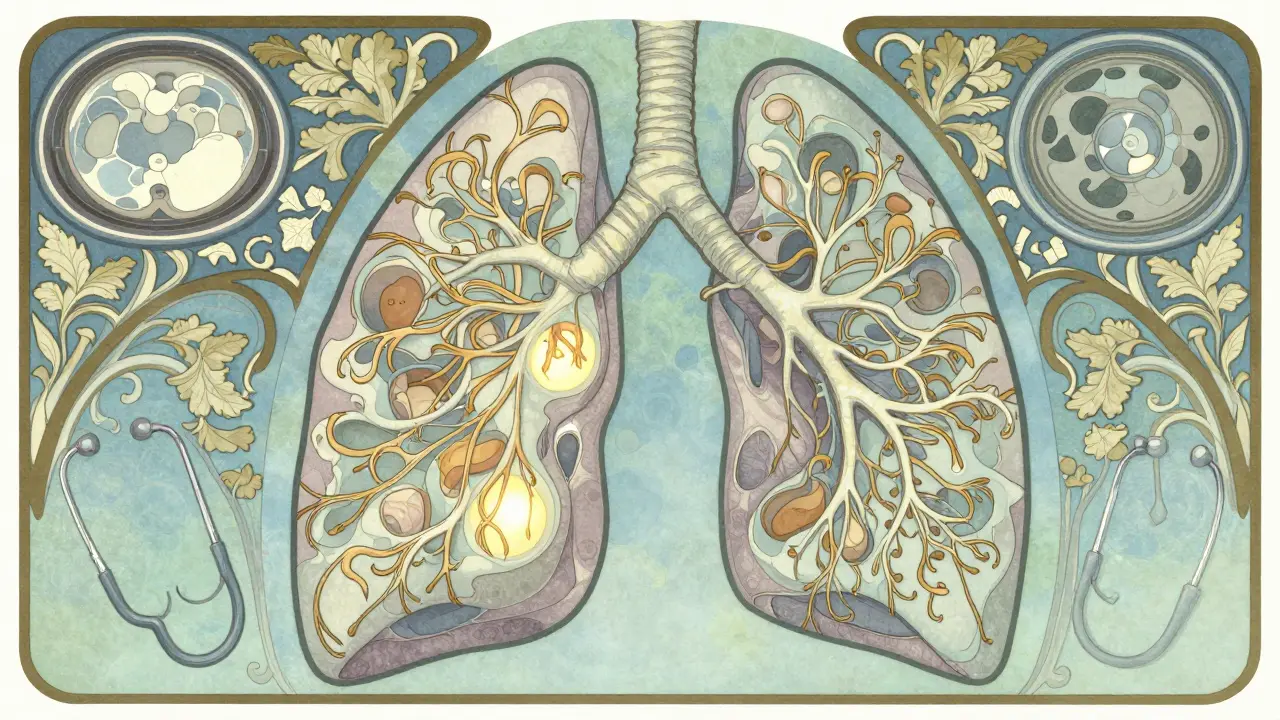
Interstitial lung disease (ILD) isn’t one single condition-it’s a group of over 200 disorders that cause progressive scarring in the lungs. This scarring, called fibrosis, happens in the interstitium, the thin tissue between the air sacs (alveoli) where oxygen enters your bloodstream. When this tissue thickens and stiffens, your lungs can’t expand properly. You don’t get enough oxygen, even when you’re at rest.
Unlike asthma or COPD, where airways narrow, ILD damages the lung’s structure itself. Once scarred, lung tissue doesn’t heal. That’s why catching it early matters more than almost anything else. The most common type is idiopathic pulmonary fibrosis (IPF), which makes up 20-30% of all ILD cases. IPF has no known cause, and without treatment, most people live only 3 to 5 years after diagnosis.
How Do You Know If You Have ILD?
Symptoms start slowly and are easy to ignore. You might think you’re just getting older or out of shape. The first sign is usually shortness of breath during activity-climbing stairs, walking to the mailbox, or carrying groceries. Over time, that breathlessness creeps into everyday moments: talking, eating, even sitting still.
Other common signs include a dry, hacking cough that won’t go away, constant fatigue, and unexplained weight loss. In advanced cases, you might notice clubbing-your fingertips becoming rounded and wider at the tips. Oxygen levels drop below 88% at rest, which means you’ll need supplemental oxygen. About 55% of people with IPF need oxygen within two years of diagnosis.
Doctors don’t diagnose ILD based on symptoms alone. A chest X-ray might show shadows, but it’s not detailed enough. The gold standard is a high-resolution CT scan (HRCT) with 1mm slices. This shows the exact pattern of scarring. But even then, misdiagnosis happens in 25-30% of cases. Many are told they have asthma, heart failure, or just “aging lungs.” On average, it takes over 11 months from first symptoms to a correct diagnosis.
What Causes the Scarring?
Not all ILD is the same. The cause changes how it behaves and how it’s treated.
- Idiopathic pulmonary fibrosis (IPF): No known cause. It’s the most aggressive form, with lung function declining 200-300 mL per year in forced vital capacity (FVC).
- Connective tissue disease-related ILD: Linked to rheumatoid arthritis, scleroderma, or lupus. These often progress slower than IPF, with 70-80% survival at five years.
- Occupational or environmental ILD: Caused by long-term exposure to asbestos, silica dust, bird droppings, or mold. These account for 15-20% of cases globally. Asbestosis, for example, progresses slower than IPF-about 100-150 mL FVC decline per year.
- Drug-induced ILD: Certain medications like chemotherapy drugs, some antibiotics, and heart medications can trigger it. Stopping the drug often leads to improvement within 3-6 months.
- Radiation-induced ILD: Happens after chest radiation for cancer. About 30-50% of patients develop permanent scarring.
- Sarcoidosis: An immune disorder that causes granulomas (clumps of inflammatory cells). Around 60-70% of cases resolve on their own within two years.
One big surprise: genetic risk plays a role. The MUC5B gene mutation, found in about 30% of people with IPF, increases the chance of developing the disease. Testing for this is now part of early risk assessment.

What Treatments Actually Work?
There’s no cure. But treatment can slow scarring and help you live better.
Since 2014, two antifibrotic drugs have changed the game: nintedanib (Ofev®) and pirfenidone (Esbriet®). Both are taken daily, and both reduce the rate of lung function decline by about half over a year. In clinical trials, patients on these drugs lost 50% less FVC than those on placebo. They don’t reverse scarring-they stop it from getting worse faster.
Side effects are real. With pirfenidone, 65% of users get sun sensitivity-some get rashes from even brief outdoor exposure. About 58% have nausea, vomiting, or loss of appetite. Nintedanib causes diarrhea in nearly half of users. Dosing adjustments and timing (taking meds with food) help manage these.
Here’s the catch: these drugs are approved mainly for IPF. For other ILD types, like sarcoidosis or connective tissue disease, they’re not always effective. New drugs are coming. In September 2023, the FDA approved zampilodib, the first new antifibrotic in nearly a decade. Early data shows a 48% reduction in lung function decline compared to placebo.
Non-Drug Treatments That Make a Difference
Medications aren’t the whole story. Pulmonary rehabilitation is one of the most powerful tools-and it’s underused. These programs run 8-12 weeks, with 24-36 supervised sessions. You get exercise training, breathing techniques, nutrition advice, and emotional support.
People who complete rehab improve their 6-minute walk distance by 45-60 meters on average. That’s not just a number-it means you can walk to the store without stopping. It means you can play with your grandkids again. About 72% of participants report moderate to significant improvement in daily life.
Oxygen therapy becomes necessary when your blood oxygen drops below 88%. Portable oxygen concentrators let people stay mobile. Many patients report feeling less anxious and more in control once they start using oxygen consistently.
Energy conservation is another key skill. Learning how to pace yourself, sit while doing chores, or use assistive devices cuts fatigue. Occupational therapy helps with this-usually 4-6 weeks of training.
What’s New in ILD Research?
Science is moving fast. Artificial intelligence is now helping radiologists read CT scans. Mayo Clinic’s AI tool correctly identified ILD subtypes in 92% of cases-better than human experts, who got it right 78% of the time.
Genetic testing is becoming routine. Researchers have identified 14 genes linked to ILD risk. Testing for the MUC5B mutation now helps predict who’s likely to have rapid progression. That lets doctors start treatment earlier.
Clinical trials are exploring new paths: stem cell therapies, drugs that target inflammation before fibrosis starts, and combination therapies. There are 9 phase 3 trials for new tyrosine kinase inhibitors and 17 stem cell studies active as of late 2023.
The biggest shift? Doctors are no longer just watching lung function. They’re listening to patients. New trial endpoints now include quality-of-life measures-how tired you feel, how much you can do, how anxious you are. That’s a win for people living with ILD every day.
Living With ILD: Real Challenges
Behind the numbers are real lives. A 2023 survey of over 1,200 ILD patients found that 78% were misdiagnosed at least once. Many were told their breathlessness was just “getting old.” That delay costs time-and lung function.
Family caregivers spend an average of 20+ hours a week helping. The biggest burdens? Managing oxygen equipment (76%) and helping with mobility (68%). Many caregivers report feeling isolated and exhausted.
Anxiety is common. About 68% of patients say fear of breathlessness keeps them from socializing. Oxygen tanks make people feel conspicuous. Some avoid going out altogether.
Cost is another hurdle. Nintedanib costs about $9,450 a month. Pirfenidone runs $11,700. Insurance often covers them, but co-pays can be thousands. Patient assistance programs exist, but navigating them is confusing.
When to See a Specialist
If you’ve had unexplained shortness of breath for more than a few weeks-especially with a dry cough-and your doctor says it’s “just aging,” push back. Ask for a referral to a pulmonologist who specializes in ILD.
Not all lung doctors are the same. Academic medical centers with dedicated ILD clinics diagnose and treat these conditions far more accurately than general hospitals. Community hospitals miss 35% more cases than specialty centers.
Don’t wait for symptoms to get worse. Early diagnosis means early treatment. And early treatment means more time doing the things you love.

12 Comments
This is why people die waiting for doctors to stop calling it 'just aging.'
lol at the 11 month diagnosis time lol
So let me get this straight - we’ve got AI outperforming radiologists, drugs that barely slow the rot, and patients still being told they’re just old? The system’s not broken. It’s designed this way.
The profound tragedy of interstitial lung disease lies not merely in its physiological deterioration, but in the existential isolation it imposes upon those who endure it. The human spirit, when confronted with the slow erosion of breath - the very essence of life - is forced into a silent negotiation with mortality. We speak of FVC decline and CT scan patterns, yet we neglect the trembling hands that reach for the oxygen concentrator at 3 a.m., the silenced laughter at family dinners, the unspoken grief of caregivers who sacrifice their own vitality to sustain another’s. This is not a medical condition; it is a societal failure to prioritize dignity over metrics.
I had a cousin with IPF. He started on nintedanib and honestly, the diarrhea was brutal. But he got to see his granddaughter graduate. That’s worth every stomach ache.
I’ve been in pulmonary rehab for six months now and it’s the only thing that’s kept me from turning into a ghost. The breathing exercises? Life-changing. The group chats at 7 p.m. after class? Even better. You don’t realize how much you miss being around people who get it - not just ‘oh that’s rough,’ but ‘I know exactly what that feels like.’ And the energy conservation tips? I started sitting while brushing my teeth. I used to stand there for 10 minutes like a statue. Now I’m just… sitting. And I’m not exhausted by 10 a.m. anymore. It’s the small things. The tiny rebellions against the disease. You don’t need a miracle drug to feel alive again - you just need someone to tell you it’s okay to move slower.
Ah yes, the grand narrative of modern medicine - we’ve replaced suffering with algorithms and pharmaceuticals that make you puke. How poetic. We’ve turned the sacred act of breathing into a data point on a graph while the world outside burns. The real fibrosis? It’s not in the lungs. It’s in our collective indifference.
I think people forget that the MUC5B mutation isn’t just some genetic glitch - it’s like your body’s got a backdoor for fibrosis. Like your lungs are secretly programmed to betray you. And then we wonder why people are scared to get tested? Imagine knowing your future is written in your DNA. That’s not science. That’s a horror movie with a co-pay.
Let’s be real - the only reason these drugs got approved is because Big Pharma realized they could charge $10k/month for something that doesn’t cure you but makes you feel like you’re still fighting. And don’t get me started on the oxygen tanks. You’re not a patient. You’re a walking billboard for corporate greed. Meanwhile, the people who actually need this stuff are stuck in insurance purgatory while CEOs take vacations in the Maldives. This isn’t healthcare. It’s a performance art piece on capitalism’s cruelty.
Wait so zampilodib is approved? Bro I read the phase 2 data and it was a mess. They used a 300m walk test as the endpoint? That’s not even real life. My aunt walked 50m before she had to sit down. And you think a 48% reduction in decline means anything if you’re still gasping for air? This is just placebo with a fancy name. Stop selling hope. Start selling results.
I’m from Johannesburg. We don’t have access to half this stuff. No AI scans. No antifibrotics. No rehab programs. My brother got diagnosed with ILD and the hospital said ‘go home and rest.’ So I made him a breathing mask from a plastic bottle and a vacuum filter. We used YouTube videos to teach him diaphragmatic breathing. He’s still here. Not because of medicine. Because we refused to let him disappear.
I’m the author of this post. Thank you all for sharing your stories - even the angry ones. I didn’t write this to be a textbook. I wrote it because I sat in a clinic for 14 months before someone listened. I’ve been on pirfenidone for two years. My cough is quieter. My oxygen levels are stable. But I still cry when I can’t carry my dog to the vet. This isn’t just about data. It’s about the quiet moments no trial measures. And if one person reads this and pushes back on their doctor? That’s the win.