For people with severe asthma, oral corticosteroids (OCS) have long been the go-to rescue when breathing gets tight. But what starts as a short-term fix often turns into a lifelong burden. Many patients describe OCS as a necessary evil-it keeps them breathing, but at a steep cost to their body and quality of life. The truth is, relying on these pills isn’t just outdated-it’s dangerous. And the good news? There are better, safer options now.
Why Oral Corticosteroids Are a Problem
Oral corticosteroids like prednisone and prednisolone work fast. They calm inflammation in the airways, reduce flare-ups, and can even keep someone out of the hospital. But that relief comes with a price tag that shows up over time-not just in dollars, but in your bones, blood sugar, mood, and heart. Studies show 93% of people with severe asthma who use OCS regularly experience serious side effects. Even short courses-just a few days-can trigger weight gain, high blood pressure, or spikes in blood sugar. Long-term use? That’s where things get worse. Osteoporosis, cataracts, glaucoma, diabetes, depression, and even adrenal insufficiency become real risks. Some patients develop these problems after only 30 days of use. And it’s not just health. The financial burden is heavy. In Italy, the cost of treating OCS-related complications in asthma patients averages €1,960 per year-nearly double what non-asthma patients pay. These aren’t hidden costs. They’re hospital visits, medications for side effects, lost workdays, and emergency care. Meanwhile, the pills themselves cost pennies. The real expense is what happens after.What Does OCS Dependence Really Mean?
Doctors don’t just hand out OCS forever. But for some patients, it’s hard to stop. OCS dependence is defined as taking these pills for six months or longer, even at low doses like 5-7.5 mg daily. It’s not laziness or noncompliance-it’s often a sign that the asthma isn’t being controlled at its root. The problem? Many patients and even some clinicians think OCS is the only tool left. But GINA guidelines, updated in 2024, clearly state: OCS should be the absolute last resort at Step 5 of asthma treatment. Before you reach for daily pills, you should try something else. And here’s the catch: frequent OCS use often means your asthma isn’t responding to inhaled steroids or other controllers. That’s not your fault. It’s a signal that your type of asthma needs a different approach-one that targets inflammation at the source.The Game Changer: Biologics
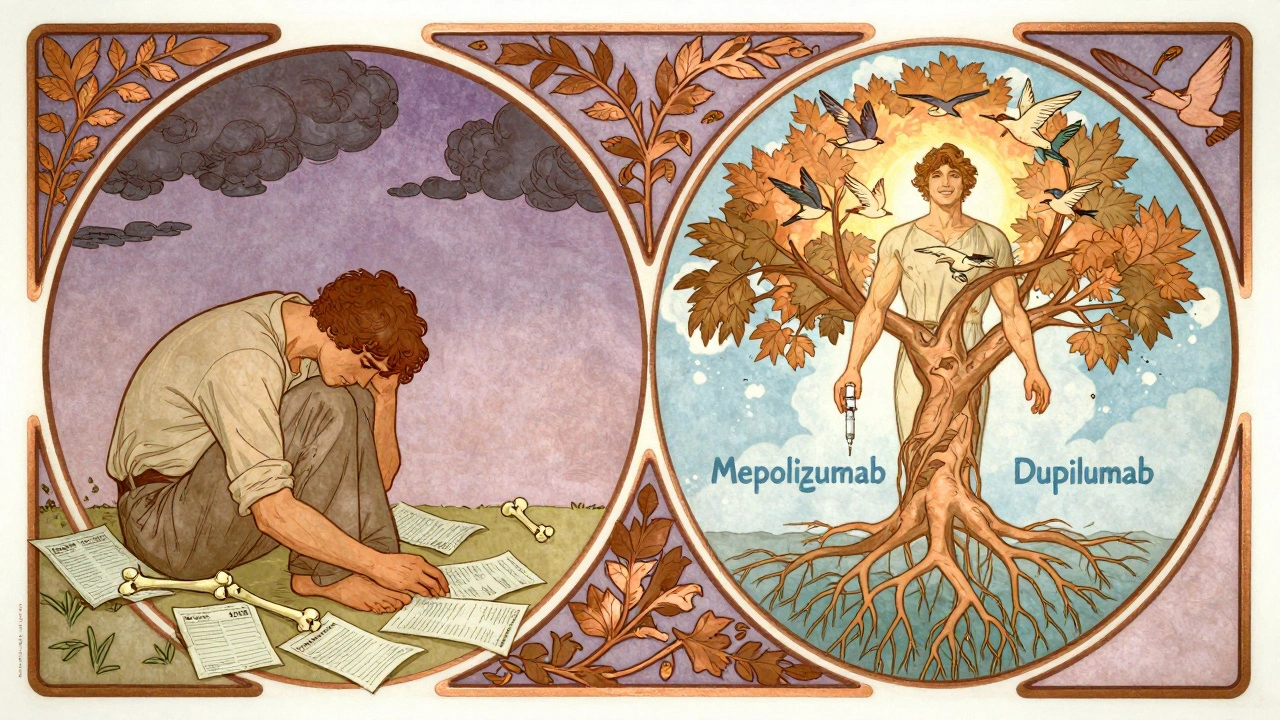
Biologics are the most powerful alternative to OCS dependence. These are injectable or IV medications that don’t just suppress inflammation-they target specific parts of the immune system driving asthma. Six biologics are approved for asthma in 2025:- Omalizumab
- Mepolizumab
- Reslizumab
- Benralizumab
- Dupilumab
- Tezepelumab
- 79% of patients on daily OCS dropped to just 31%
- Average daily OCS dose fell by 4.7 mg
- Exacerbations dropped from 4.1 per year to 0.8
- Hospitalizations fell from 0.4 to 0.06 per year
Are Biologics Worth the Cost?
Yes. And here’s why. Biologics cost more upfront. A single dose can run $10,000-$30,000 per year. But OCS? The pills themselves are cheap. The real cost is what happens afterward. A 2023 analysis in Advances in Therapy calls these the “shadow costs”: diabetes meds, bone density scans, heart treatments, mental health care, missed work, and emergency visits. When you add them up, biologics pay for themselves in under two years for many patients. And access is improving. In June 2024, major inhaler manufacturers capped out-of-pocket costs at $35 per month for inhalers. While this doesn’t cover biologics yet, it shows a shift in policy. More insurers are starting to cover biologics for OCS-dependent patients because the long-term savings are undeniable.Other Alternatives-What Works and What Doesn’t
Biologics aren’t the only option, but others have limits. Bronchial thermoplasty uses heat to reduce excess airway muscle. It’s done in three sessions via bronchoscopy. Some patients see fewer flare-ups and better quality of life. But in the six weeks after treatment, asthma symptoms often get worse. It’s only considered for those who’ve tried everything else-and it’s not widely available. What about vitamins? High-dose vitamin D? Studies show it doesn’t help. A 2021 review found no improvement in exacerbations or control, even in people with low vitamin D levels. Same with omega-3s, probiotics, or herbal remedies. No solid evidence supports them for severe asthma. The bottom line: if you’re on daily OCS, don’t waste time on supplements that don’t work. Focus on what does.
How to Start the Transition
Switching from OCS to biologics isn’t instant. You can’t just stop steroids cold. That’s dangerous-it can trigger adrenal crisis. The process looks like this:- Get tested for type 2 inflammation (blood eosinophils, IgE, FeNO)
- Work with your pulmonologist to confirm you’re a candidate
- Start the biologic while slowly reducing OCS
- Monitor symptoms, lung function, and side effects every 3-6 weeks
- Adjust the OCS taper based on how you respond


16 Comments
bro i was on prednisone for 8 months straight and my face looked like a balloon 🤡 my doctor just shrugged and said 'at least you're not in the hospital'... like thanks i guess?
i cried reading this. i haven't missed a day of work in 14 months since starting dupilumab. my kid finally got to go to the zoo without me being scared i'll collapse in the parking lot. thank you for writing this.
the fact that we still treat asthma like a 1990s problem is criminal. biologics aren't 'experimental'-they're the logical next step. if your doctor hasn't mentioned them, find a new one.
let’s be real-oral steroids are the pharmaceutical equivalent of duct tape on a leaking submarine. sure, it stops the water for now, but you’re just buying time until the whole damn hull gives out. biologics? they’re the fucking submarine repair crew with a blueprint.
the fact that we’re still debating this in 2025 is a national embarrassment. we’ve got precision medicine sitting on the shelf while people get osteoporosis from pills cheaper than their morning coffee.
and don’t even get me started on the 'vitamin D fixes everything' crowd. no, Karen, your turmeric latte isn’t reducing your eosinophils. stop googling and go see a pulmonologist.
the real tragedy? patients are terrified to ask for biologics because they think it’s 'too much' or 'too expensive.' but the real cost is your spine crumbling, your mood evaporating, your job slipping away. that’s not a trade-off-it’s a slow-motion suicide.
if you’re on daily OCS, you’re not 'managing' asthma-you’re surviving it. and survival isn’t living.
we need to stop glorifying endurance. we need to stop praising people who 'tough it out' on prednisone like it’s some kind of badge of honor. it’s not resilience. it’s neglect.
biologics don’t just reduce exacerbations-they restore personhood. you get to sleep through the night. You get to hold your grandkid without wheezing. You get to laugh without gasping.
the insurance hurdles? real. the access gaps? criminal. but the data? unassailable. if you’re eligible, fight for it. scream for it. email your senator. write your congressman. your lungs are worth it.
and if you’re a clinician reading this-stop waiting for perfect guidelines. start having the conversation. your patient might not survive another 6 months on 10mg daily.
we’re not talking about 'options' anymore. we’re talking about justice.
as an Aussie who’s seen this play out in our public health system, I can confirm: biologics save lives and reduce hospital loads. we’ve got them covered under PBS now for qualifying cases. if you’re in the US and struggling with access, reach out-there are patient advocacy groups that help navigate this.
also, side note: the 'vitamin D myth' is everywhere here too. people swear by it. it’s like the asthma version of 'I drank celery juice and my cancer vanished.'
you’re all missing the point. this isn’t about asthma. it’s about how medicine prioritizes profit over people. biologics cost $30k a year? great. now make a generic version. stop letting Big Pharma hold patients hostage while they milk the system. the science is here-capitalism isn’t.
my mom was on prednisone for 11 years. she lost her bones, her joy, her ability to walk without pain. when she switched to mepolizumab, she cried the first time she carried groceries without stopping to catch her breath. she’s 72 now. she dances at my wedding next month. this isn’t medicine. this is magic.
who’s really behind this? the pharmaceutical industry? they’re pushing biologics because they make billions. but what if the real solution is just cleaning the air? why aren’t we talking about pollution? why aren’t we holding factories accountable? this feels like a distraction.
as an American who’s had to fight insurance for 14 months just to get a biologic approved, I’m tired of hearing how 'it pays for itself.' it didn’t pay for me. I lost my job. I maxed out my credit cards. My daughter had to skip her birthday party because I couldn’t afford gas to get to the clinic. So don’t tell me it’s affordable. It’s not. Not for most of us.
if you’re on OCS and reading this-please, please, please ask your doctor about FeNO testing. it’s a simple breath test. no needles. no cost. it tells you if you’re a candidate for biologics. I had no idea mine was elevated until I asked. changed everything.
also-don’t wait for your doctor to bring it up. be the patient who says: 'I want to try a biologic. Can we start the process?'
you deserve better. and you’re not being difficult for asking.
my brother was on 20mg daily. now he’s off steroids, hiking in the Rockies, and sleeping through the night. he said the first time he didn’t wake up coughing, he felt like he’d been given back his life. that’s not science-that’s a miracle.
biologics are great and all but why is it that only rich people get them? i work two jobs and my insurance says 'no' because i'm not 'severe enough'... but i'm on 7.5mg a day and i can't even climb stairs without stopping. who decides what 'severe' means? the drug reps?
the real question is not whether biologics work, but whether we as a society have the moral courage to fund them. we spend billions on war, on surveillance, on luxury cars for CEOs. but when a child needs an injection to breathe, we say 'it’s too expensive.'
we are not a society that values breath. we are a society that values profit.
ask yourself: if your mother had asthma, would you let her die slowly on prednisone because of bureaucracy?
i’ve been on OCS for 9 years. i don’t want to be. but i’m scared to stop. what if i die? what if i can’t breathe? no one talks about that fear. they just say 'try biologics.' but what if they don’t work? what if i’m stuck forever?
the clinical pathway outlined in this post is exemplary. however, the lack of standardized, evidence-based tapering protocols remains a critical gap in implementation. the EOS Network and GINA must prioritize the development of a consensus algorithm for OCS reduction in conjunction with biologic initiation. Without this, even the most effective therapies risk suboptimal outcomes due to inappropriate dosing schedules. I recommend that all centers adopt a multidisciplinary tapering team including pulmonologists, endocrinologists, and pharmacists.
thank you for this. i’ve been trying to get my clinic to adopt this approach for years. the biggest barrier isn’t the science-it’s inertia. we’ve been doing it the old way for so long, we forget there’s another path. your post gave me the courage to bring it up at our next grand rounds.