When a drug leaves the lab and enters the real world, it faces heat, humidity, light, and time-none of which care about its intended shelf life. That’s why stability testing isn’t just paperwork. It’s the last line of defense between a patient getting a safe, effective medicine and one that’s broken down, useless, or even dangerous.
Why Stability Testing Exists
Every pill, injection, or inhaler you take has a shelf life. But that number-12 months, 24 months, 3 years-doesn’t come from guesswork. It’s the result of months, sometimes years, of controlled stress tests. The goal? To see how the drug changes over time under real-world conditions. If a tablet crumbles in 40°C heat or a liquid turns cloudy after six months in a warm warehouse, that’s a problem. Stability testing catches those issues before the product hits the market. The global standard for this comes from ICH Q1A(R2), a guideline developed in the 1990s by regulators from the U.S., Europe, and Japan. It’s not optional. The FDA, EMA, Health Canada, and others all require it. If you skip it, your drug won’t get approved. And if you get it wrong after launch? You could face a recall, a warning letter, or worse.Temperature and Humidity: The Core Conditions
Stability testing isn’t one-size-fits-all. It’s broken into three main categories, each with exact temperature and humidity rules.- Long-term testing: This is the real-time clock. It shows how the drug behaves under normal storage conditions. There are two accepted setups: 25°C ± 2°C with 60% RH ± 5% RH, or 30°C ± 2°C with 65% RH ± 5% RH. Which one you pick depends on where the drug will be sold. If it’s going to tropical markets like India or Brazil, you go with 30°C/65% RH. For cooler regions like Canada or Northern Europe, 25°C/60% RH is fine. You need at least 12 months of data before you can submit for approval in the U.S. Europe allows 6 months under certain conditions, but that can delay global launches.
- Accelerated testing: This is the stress test. You push the drug hard to predict how it’ll behave over years. The rule is simple: 40°C ± 2°C and 75% RH ± 5% RH for six months. This isn’t meant to be realistic-it’s meant to accelerate degradation. If the drug fails here, you know you’ve got a problem. It’s not a substitute for long-term data, but it’s your early warning system.
- Intermediate testing: This is the middle ground. You only run this if your long-term study is at 25°C and the accelerated test showed a significant change. Then you test at 30°C/65% RH for six months to bridge the gap. It’s not always required, but when it is, it can save you from a costly failure later.
Refrigerated and Frozen Products
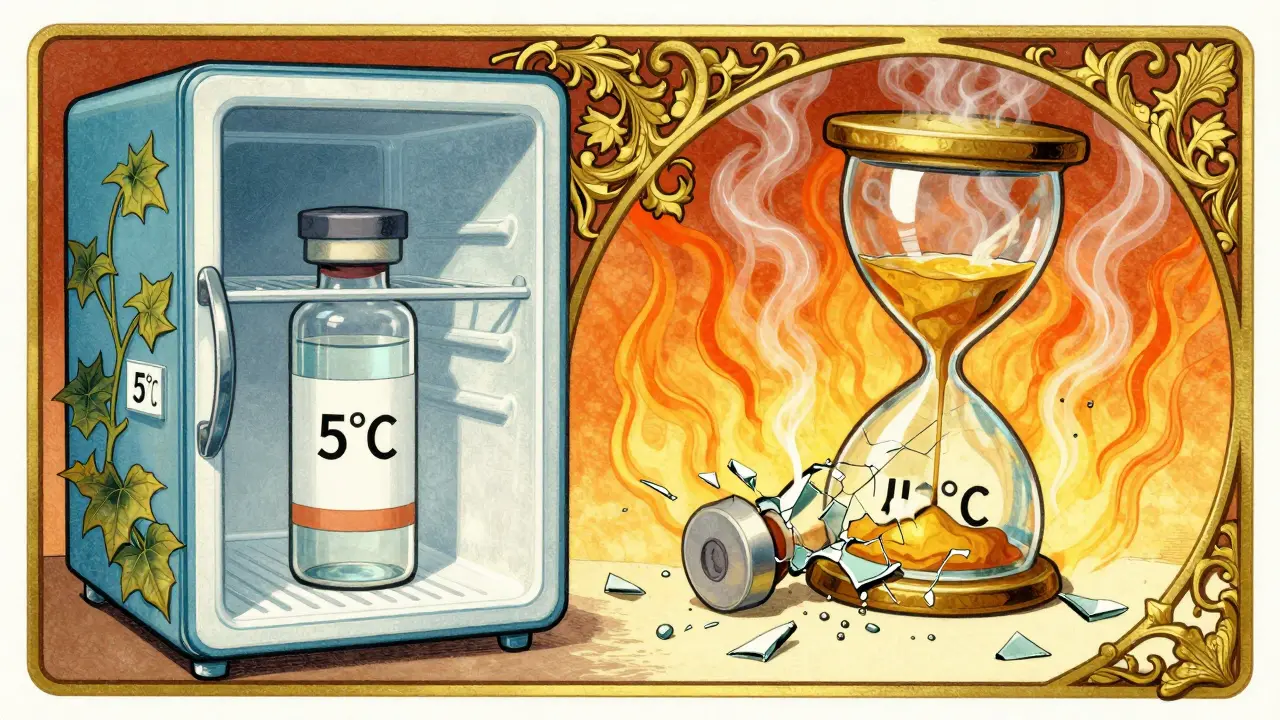
Not all drugs are stored at room temperature. Insulin, vaccines, and many biologics need to stay cold. For those, the rules change.- Long-term: 5°C ± 3°C. This is the standard fridge temperature. You test for at least 12 months.
- Accelerated: Here’s the twist. Instead of 40°C, you test at 25°C ± 2°C with 60% RH ± 5% RH for six months. Why? Because freezing and thawing are the real enemies of biologics-not heat. So you simulate the worst-case scenario: a vaccine sitting in a warm delivery truck.
Time: How Long Do You Test?
Testing isn’t a one-time event. You check the drug at specific intervals: 0, 3, 6, 9, 12, 18, 24, and 36 months. The early points (3, 6, 9 months) are critical because that’s when most changes happen. If a drug starts degrading at month 6, you need to catch it before it hits month 12. The testing schedule isn’t arbitrary. It’s based on how fast the drug breaks down. A simple tablet might be stable for 3 years, so you test every 6 months after year one. A complex biologic? You might test every month for the first year. The goal is to capture the trend-not just a snapshot.Real-World Challenges
Sounds simple, right? It’s not. In a 2023 survey of pharmaceutical professionals, 78% reported at least one temperature excursion in their stability chambers during a 12-month study. One degree outside the ±2°C range can invalidate the whole test. That means restarting months of work. Humidity control is even trickier. In dry climates, keeping 65% RH stable requires expensive humidification systems. And if your chamber has uneven airflow? One shelf might be 26°C while another is 23°C. That’s not acceptable. Chambers must be mapped and qualified before use. Then there’s the ambiguity of “significant change.” ICH Q1A(R2) doesn’t define it numerically. Is a 3% drop in potency a problem? What about a color change? Different regulators interpret this differently. One company’s minor issue is another’s recall trigger. That subjectivity causes delays, legal battles, and lost revenue.What’s Changing in 2026?
The ICH Q1A(R2) guideline is 20 years old. It was designed for tablets and capsules, not mRNA vaccines or antibody-drug conjugates. Today’s drugs are more sensitive. A single freeze-thaw cycle can ruin a lipid nanoparticle. Standard 40°C tests don’t capture that. The FDA is running pilot programs using real-time monitoring tools (PAT) to predict stability without waiting years. Some companies are already using predictive models-running tests at 50°C, 60°C, even 80°C-to forecast degradation in weeks instead of months. But regulators are cautious. In 2022, the EMA rejected eight model-based stability submissions because they didn’t meet traditional standards. The next update, possibly Q1F in late 2024, will likely address these new products. Until then, companies are stuck between old rules and new science.
What Happens If You Get It Wrong?
In 2021, Teva Pharmaceuticals had to recall 150,000 vials of Copaxone® because their stability tests didn’t catch aggregation under 40°C heat. Patients got a drug that was less effective. In 2022, Amgen received an FDA warning letter after their monoclonal antibody product degraded during shipping in hot climates. These aren’t rare. The FDA issued 27 warning letters in 2022 alone for stability testing failures. That’s not just bad science-it’s a patient safety risk.Who Does This Work?
Large pharma companies have entire departments dedicated to stability testing. They spend $185,000 to $275,000 per product on full testing programs. Smaller biotechs outsource to CROs like WuXi AppTec or Charles River Laboratories. But even with outsourcing, the process is slow. On average, stability data delays product launches by 9-12 months. The people running these tests? Stability analysts. They’re not lab techs. They’re statisticians, environmental engineers, and regulatory experts rolled into one. They run ANOVA models, interpret chromatograms, and write 500-page dossiers. Their work is quiet, repetitive, and critical.Bottom Line
Stability testing isn’t about checking boxes. It’s about ensuring that every dose a patient takes is as good as the day it was made. The temperature and time conditions in ICH Q1A(R2) are strict for a reason. They’re based on decades of data, real failures, and patient harm. But the world is changing. New drugs demand new rules. Until those rules arrive, companies must follow the existing ones-perfectly. Because in pharmaceuticals, there’s no second chance to get it right.What are the standard temperature and humidity conditions for long-term stability testing?
The ICH Q1A(R2) standard allows two options: 25°C ± 2°C with 60% RH ± 5% RH, or 30°C ± 2°C with 65% RH ± 5% RH. The choice depends on the target market’s climate zone. For tropical regions, 30°C/65% RH is required. In temperate regions, 25°C/60% RH is acceptable. At least 12 months of data under these conditions must be available for regulatory submission in the U.S.
Why is accelerated testing done at 40°C and 75% RH?
The 40°C/75% RH condition is designed to simulate extreme environmental stress, like a drug being stored in a hot warehouse or shipped in a non-climate-controlled truck. It’s not meant to reflect normal conditions-it’s a predictive tool. Under this stress, most small-molecule drugs degrade about four times faster than at 25°C/60% RH, allowing scientists to estimate shelf life in just six months instead of years.
Do refrigerated drugs follow the same stability rules as room-temperature drugs?
No. Refrigerated drugs are tested at 5°C ± 3°C for long-term stability. Their accelerated test is done at 25°C/60% RH-not 40°C. This is because biologics, vaccines, and injectables are more vulnerable to freezing and thawing cycles than heat. Testing at 40°C wouldn’t reflect their real-world risks. WHO guidelines and FDA recommendations both support this adjusted approach.
What happens if a stability chamber has a temperature excursion?
Any temperature deviation outside ±2°C or humidity outside ±5% RH can invalidate the entire study. If this happens, you must document the event, assess its impact on the samples, and potentially restart the test. In 2023, 78% of pharmaceutical professionals reported at least one such incident during a long-term study. This is why chambers require rigorous qualification and continuous monitoring.
How does ICH Q1A(R2) handle new drug types like mRNA vaccines or biologics?
The current ICH Q1A(R2) guideline doesn’t fully address complex products like mRNA vaccines, monoclonal antibodies, or antibody-drug conjugates. These drugs degrade in ways traditional tests don’t capture-like freeze-thaw damage or protein aggregation. Regulators are aware, and ICH is working on an update (likely Q1F in late 2024). Until then, companies must use risk-based approaches, sometimes supplementing ICH with custom protocols approved by regulators.
Can predictive modeling replace physical stability testing?
Some companies use predictive models-testing at 50°C-80°C-to forecast stability in weeks instead of years. But regulators like the FDA and EMA still require real-time data for approval. In 2022-2023, the EMA rejected eight submissions that relied solely on modeling. While models are useful for early screening, physical testing remains mandatory for regulatory filings. The future may shift toward hybrid approaches, but not yet.


11 Comments
This is WHY I love pharma science 🤓🌡️ One degree off and BOOM - whole study invalid? Wild. But also... sooo necessary. Patients deserve this level of care.
I’ve seen stability chambers go haywire during summer power surges. It’s terrifying how fragile these systems are. Glad someone’s documenting it.
i just learned that biologics dont use 40c for accel testing? that makes so much sense. i always thought it was one size fits all. thanks for clarifying!
The part about 78% of labs having temp excursions? That’s not a fluke - that’s a systemic issue. We need cheaper, smarter monitoring tools. Not everyone has $200k for a qualified chamber. This isn’t just science - it’s equity.
The assertion that ICH Q1A(R2) is '20 years old' is misleading. It was published in 1997 and reaffirmed in 2003. To imply it’s outdated without acknowledging its foundational rigor is scientifically irresponsible. Moreover, the term 'significant change' is explicitly defined in ICH Q6A, not Q1A. You're conflating guidelines.
I’ve worked in a CRO in Bangalore where we tested insulin under 5°C for 24 months. The humidity control was a nightmare - we used industrial humidifiers and still had 5% swings. It’s insane how much manual labor goes into this. Hats off to the analysts.
So we spend $250k per drug to make sure it doesn’t turn into soup… and then someone leaves it in a hot car for 2 hours? Yeah, I guess we’re all just waiting for the next recall.
It’s funny how we treat drugs like they’re perfectly stable objects. But they’re not. They’re living chemistry. Maybe the real question isn’t how to test them better - but whether we’re trying to control nature too hard.
bro the 40c test is wild but it works. we did a 60c test on a new tablet last year and saw degradation in 72 hours. saved us 18 months. regulators still made us do the full 12mo tho. so frustrating.
Let me be real - stability testing is the unsung hero of every pill you take. No one cheers for the analyst running ANOVA at 2am. But if they miss a 3% potency drop? Someone dies quietly in a nursing home. This isn’t bureaucracy. It’s a moral contract.
I’ve been in this field for 15 years. The real problem isn’t the guidelines - it’s that we still use 1990s lab equipment to test 2020s drugs. We’re using slide rules to navigate a jetliner.