Immunosuppressive Therapy: What It Is, How It Works, and What You Need to Know
When your immune system turns against your own body—attacking healthy tissues, rejecting a transplanted organ, or overreacting to harmless substances—it’s not being helpful. That’s where immunosuppressive therapy, a medical approach that deliberately reduces immune system activity to prevent damage. Also known as immune suppression treatment, it’s a lifeline for people with autoimmune diseases like lupus or rheumatoid arthritis, and for those who’ve received a kidney, liver, or heart transplant. Without it, the body would destroy the new organ or keep inflaming joints, skin, or organs. But this isn’t a simple fix—it’s a balancing act. Too much suppression leaves you open to infections; too little means your immune system fights back.
Drugs used in immunosuppressive therapy, a targeted medical strategy to dampen immune responses. Also known as immunosuppressants, it include corticosteroids, calcineurin inhibitors like cyclosporine, and newer agents like mycophenolate. These aren’t just pills you pop—they’re carefully timed, monitored, and adjusted based on blood tests, organ function, and infection risk. For example, someone on a transplant regimen might need blood levels checked weekly at first. Meanwhile, patients with MS or Crohn’s disease might use these drugs long-term, but with extra caution for things like skin cancer or shingles. The goal isn’t to shut down immunity completely—it’s to quiet the noise so your body doesn’t attack itself.
What you won’t find in most brochures? The real trade-offs. A 2022 study in the Journal of Transplantation showed that 1 in 4 transplant patients on long-term immunosuppressants developed a serious infection within three years. And for people with lupus, some drugs reduce flare-ups but raise diabetes risk. That’s why knowing your options matters. You might be on tacrolimus now, but could belimumab or sirolimus work better for you? Are there lifestyle tweaks—like avoiding raw sprouts or undercooked meat—that reduce infection risk without changing your meds? These aren’t theoretical questions. They’re daily realities for hundreds of thousands.
Below, you’ll find real-world guides on how these drugs interact with other conditions—like kidney failure or liver function—and how side effects like diarrhea, heart rhythm issues, or nerve damage show up in practice. You’ll see how genetic factors affect drug safety, how to travel safely with these prescriptions, and how to interpret the numbers behind risk and benefit. This isn’t just theory. It’s what people actually deal with when they’re on immunosuppressive therapy—and how to manage it without losing quality of life.
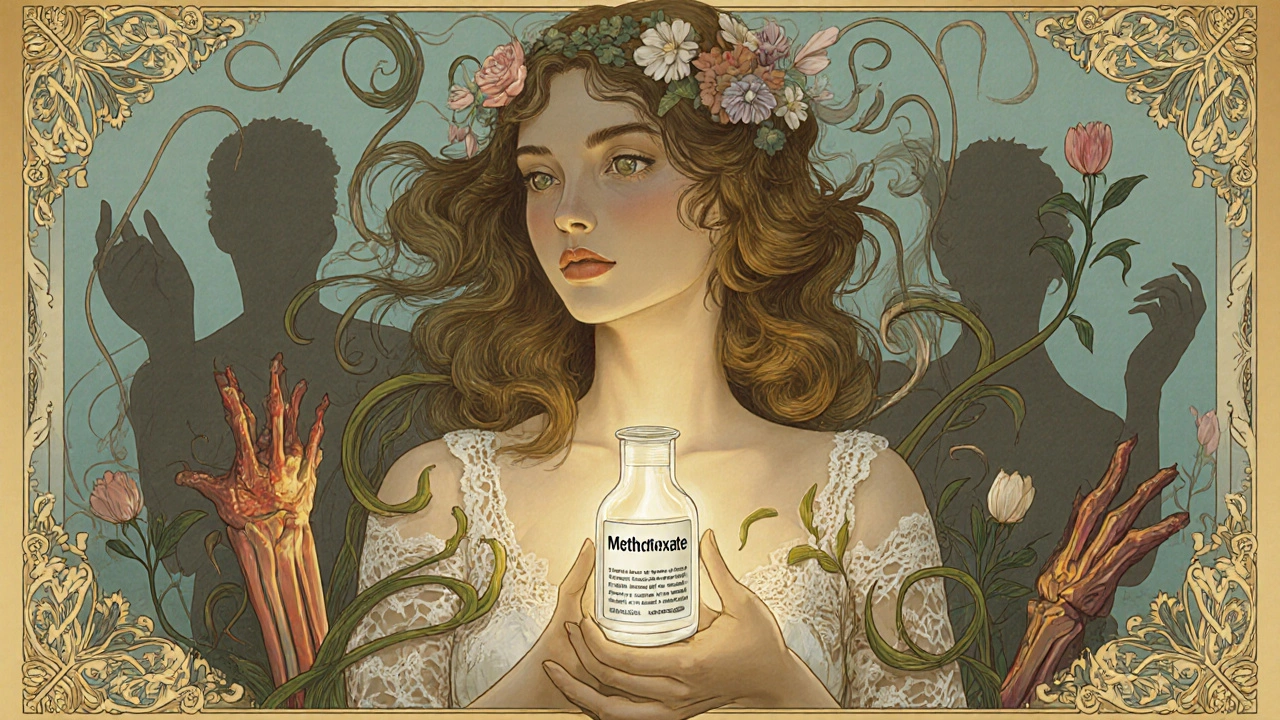
DMARDs and Biologic Medications: What You Need to Know About Immunosuppressive Therapy
DMARDs and biologic medications are essential for managing autoimmune diseases like rheumatoid arthritis. They don't just ease pain-they stop joint damage. Learn how they work, their risks, costs, and what to expect when starting treatment.
© 2026. All rights reserved.
