Rheumatoid Arthritis: Causes, Treatments, and How Medications Help
When your body turns against itself, it’s called an rheumatoid arthritis, a chronic autoimmune disease where the immune system mistakenly attacks the lining of joints, causing pain, swelling, and long-term damage. Also known as RA, it doesn’t just hurt your hands or knees—it can wear down your energy, your sleep, and your sense of control over your own body. Unlike regular joint wear and tear, rheumatoid arthritis flares up without warning, often symmetrically—both wrists, both ankles, both elbows. It’s not just aging. It’s your immune system on fire.
This condition doesn’t live in isolation. It connects to autoimmune disease, a group of disorders where the immune system attacks healthy tissue, including lupus, psoriasis, and type 1 diabetes. People with rheumatoid arthritis often have higher risks for heart disease, lung issues, and even depression because inflammation doesn’t stay in the joints—it spreads. That’s why treatment isn’t just about painkillers. It’s about stopping the attack before it damages your organs.
Medications for rheumatoid arthritis fall into clear categories. There are anti-inflammatory drugs, like NSAIDs and corticosteroids, that reduce swelling and ease pain but don’t stop the disease. Then there are disease-modifying drugs, including methotrexate, sulfasalazine, and biologics, that slow or halt joint destruction by targeting the immune system’s overactive signals. These aren’t quick fixes—they take weeks or months to work, but they’re the only things that can keep you moving years down the line. Some people need combinations. Others try newer options like JAK inhibitors when older drugs fail.
What you won’t find in most doctor’s offices is the full picture of how these drugs interact with your liver, kidneys, or even your gut. That’s why posts here cover side effects you won’t hear about in brochures—like how certain arthritis meds can trigger heart rhythm issues, or how long-term steroid use affects bone density. You’ll see real comparisons between drugs, how to manage nausea or fatigue from treatment, and what to do when your current plan stops working.
This isn’t about guessing what works. It’s about knowing what’s been tested, what’s safe for your body type, and what to ask your doctor next. Whether you’re just diagnosed or have been fighting this for years, the articles below give you the details you need—not the marketing fluff. You’ll find guides on balancing meds with diet, spotting early signs of complications, and how to travel with injectables or IV treatments. No fluff. No jargon. Just what actually helps.
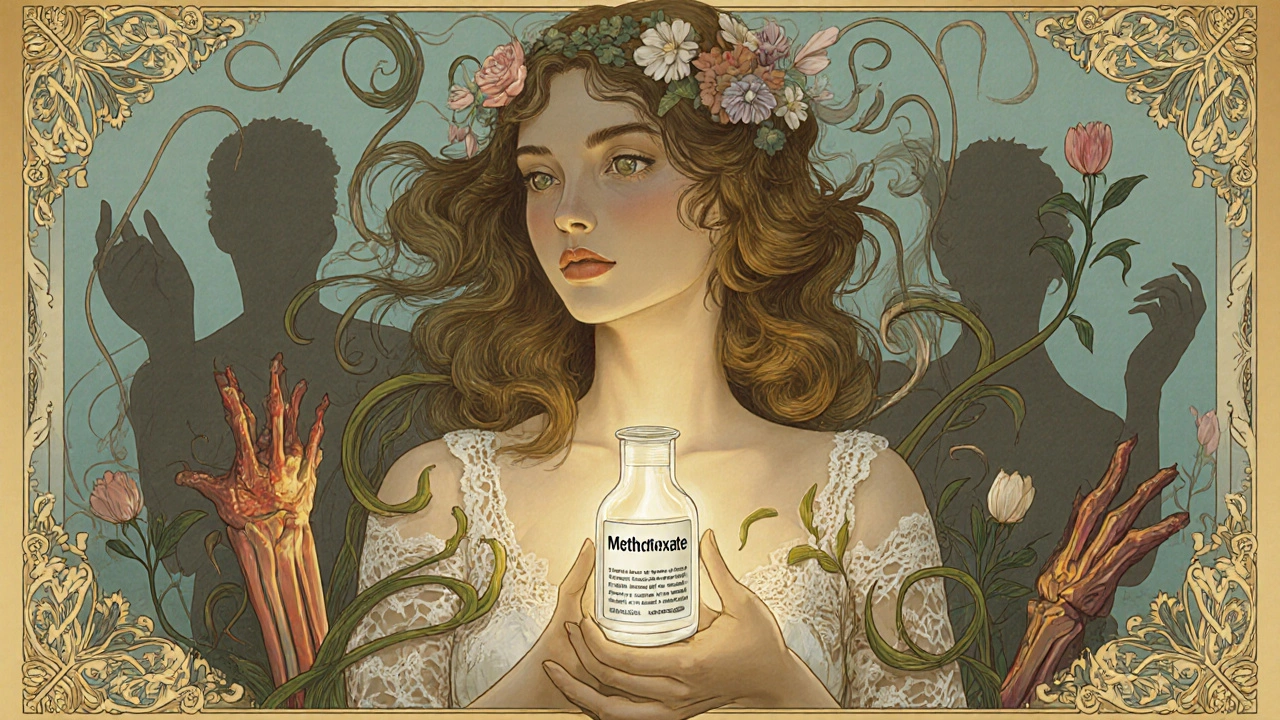
DMARDs and Biologic Medications: What You Need to Know About Immunosuppressive Therapy
DMARDs and biologic medications are essential for managing autoimmune diseases like rheumatoid arthritis. They don't just ease pain-they stop joint damage. Learn how they work, their risks, costs, and what to expect when starting treatment.
© 2026. All rights reserved.
