Swallowing issues: causes, signs, and what to do
Having trouble swallowing is scary and more common than you think. It can mean something minor, like a sore throat, or something serious, like a stroke or nerve problem. Know the signs so you can act fast: coughing or choking while eating, food sticking in your throat, drooling, hoarse voice, unexplained weight loss, or frequent chest infections.
Common causes
Swallowing problems can come from many places. Neurological issues such as stroke, Parkinson’s, or dementia often affect the muscles that move food. Acid reflux can inflame the throat and make swallowing painful. Mouth or throat infections, a tightening or narrowing of the esophagus, and tumors also cause trouble. Some medicines dry your mouth or slow movement in the gut — that can make swallowing harder too. Older adults and people after surgery often have short term trouble swallowing.
What to do now: safety, tests, and treatment
If someone can’t breathe, make sounds, or turns blue, call emergency services right away. For less dramatic but ongoing trouble, try simple safety steps: sit upright at meals, take small bites, chew slowly, and sip small sips of thickened liquids instead of thin ones. Avoid talking while eating and cut food into small pieces.
See your doctor if swallowing problems last more than a few days, get worse, or cause weight loss. A clinician may refer you to a speech-language pathologist who does bedside swallowing checks and teaches exercises. Tests that help pinpoint the problem include a modified barium swallow (video X‑ray while you swallow), a fiberoptic endoscopic evaluation of swallowing (FEES), and endoscopy to look inside the throat and esophagus. Depending on the cause, cardiologists, neurologists, ENT doctors, or gastroenterologists may join your care.
Treatment depends on the cause. Muscle-strengthening exercises and technique changes can help many people. Treating reflux, infections, or inflammation often eases swallowing. If saliva control is an issue, simple hygiene or medication may help. Severe cases that risk choking or malnutrition sometimes need feeding tubes while healing or when long term support is needed. Your care team will balance risks and quality of life when suggesting options.
At home, keep a food and symptom diary — note what textures and foods cause trouble and when symptoms show up. Bring that info to appointments. If you take medicines that dry the mouth or change movement, ask your clinician whether alternatives exist. Swallowing issues are treatable in many cases, and early action often prevents complications. Learn about related topics and medications on SecureTabsPharm to prepare for conversations with your provider.
Caregivers should help by watching meal pace, offering verbal cues, and checking for signs of aspiration like wet voice after swallowing. Try chin-tuck or double-swallow techniques shown by a speech therapist. Commercial thickening powders or natural options like mashed banana can change liquid speed, but ask a clinician before trying them. If weight drops or coughing during sleep appears, report it. Small, regular meals often work better than large plates. Stay observant and patient.
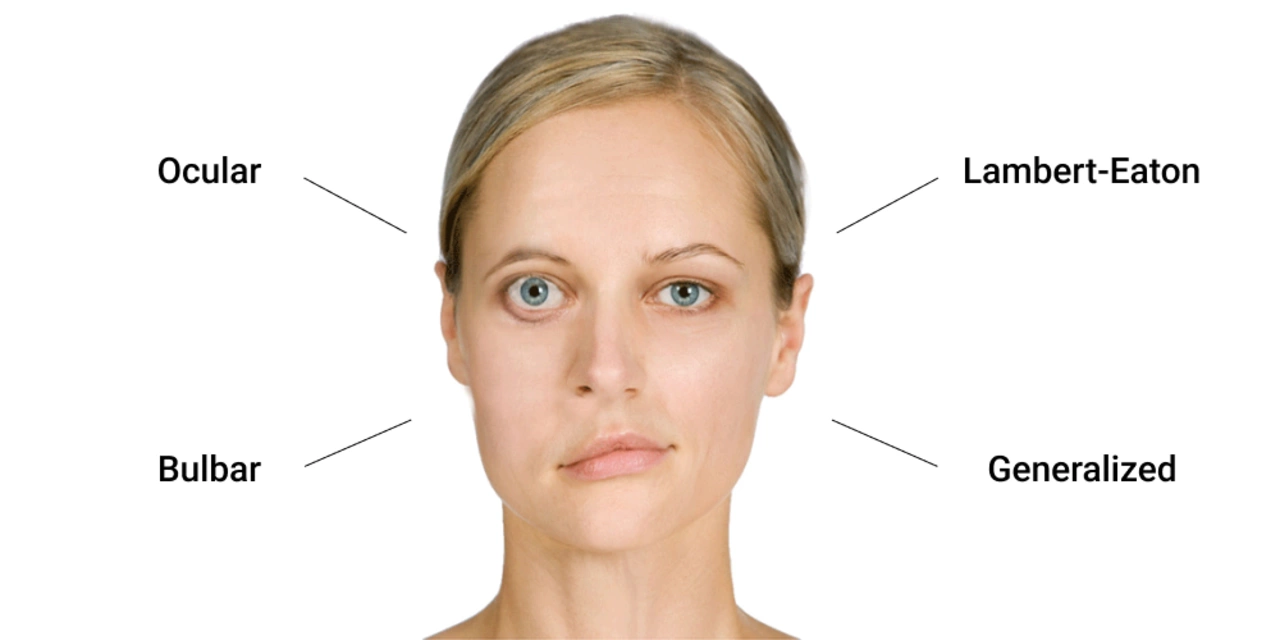
Myasthenia Gravis and Swallowing Issues: Tips for Easier Eating
Myasthenia Gravis has caused some swallowing issues for me, which can make eating a challenge. In my latest blog post, I share some helpful tips that have made eating easier and more enjoyable. I discuss the importance of sitting upright, taking smaller bites, and chewing thoroughly. Additionally, I emphasize the benefits of staying hydrated and seeking professional guidance from a speech therapist. Check out my post to learn more about managing swallowing issues related to Myasthenia Gravis.
© 2026. All rights reserved.
