Every time you pick up a prescription, you get a label. It looks simple - just a few lines of text, some numbers, maybe a logo. But that label is your lifeline. It tells you what you’re taking, why, and how to take it safely. Yet most people don’t know what every part means. And that’s dangerous. Around 1.5 million medication errors happen every year in the U.S. alone, and many of them come from misreading or misunderstanding the label. You don’t need to be a pharmacist to understand it. Here’s what each part really means - and why it matters.
Your Name - It’s Not Just for Show
The first thing on the label? Your name. It seems obvious, but this is one of the biggest safety checks in the whole system. Pharmacies fill hundreds of prescriptions a day. A mix-up between ‘John Smith’ and ‘Jon Smith’ might seem unlikely, but it happens. That’s why every label has your full name. If your name is wrong, don’t take the pills. Call the pharmacy immediately. A mismatch here can lead to someone else’s medication - and that could be life-threatening. This isn’t bureaucracy. It’s your protection.
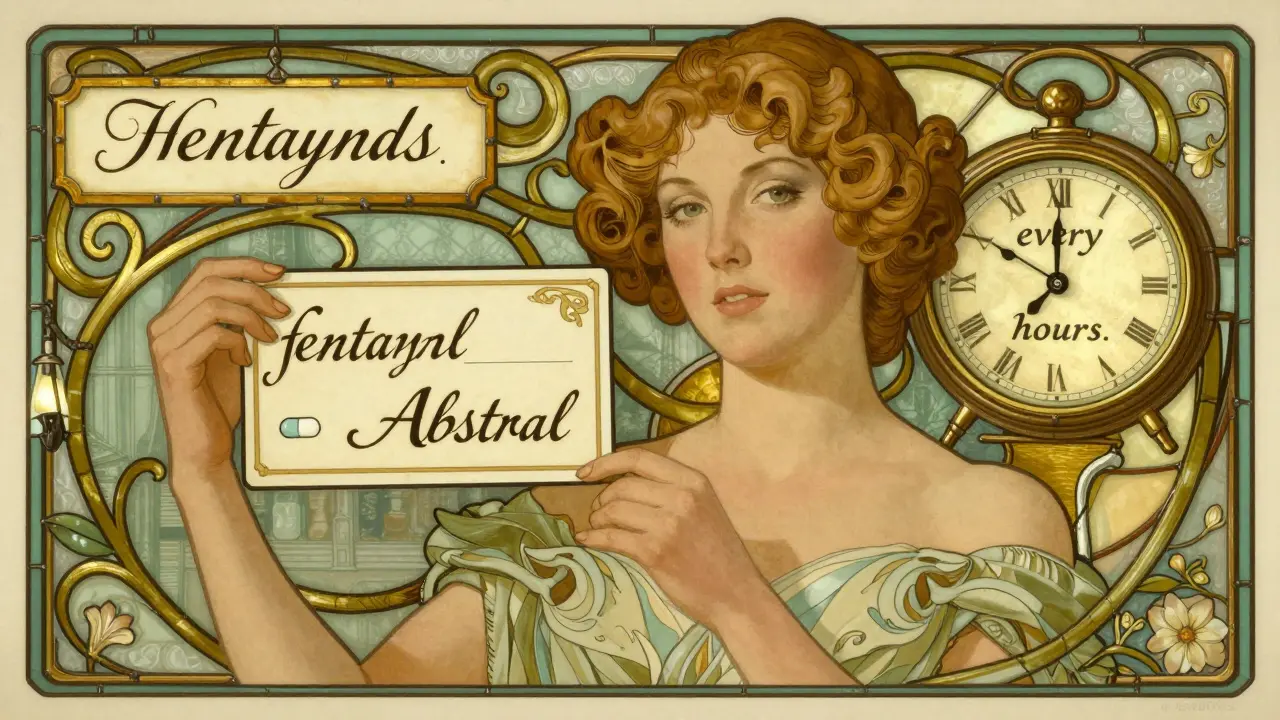
The Medication Name - Brand vs. Generic
You’ll see two names: one big and fancy, another plain and simple. The big one is the brand name - like Abstral. The smaller one underneath is the generic name - fentanyl. The generic name tells you the actual active ingredient. That’s what your body reacts to. Brand names change depending on who makes it. Generic names don’t. Knowing the generic name helps you recognize the same drug if you switch pharmacies, get a refill, or see it listed in a doctor’s note. It also helps you avoid taking two versions of the same thing. For example, if you’re on both brand-name and generic ibuprofen, you could accidentally double your dose.
Dosage Strength - How Much Is in Each Pill?
This tells you the exact amount of medicine in each tablet, capsule, or milliliter. You might see something like “100 mcg” or “500 mg.” That’s not a suggestion. That’s the dose. Taking more than what’s written can cause overdose. Taking less might mean the medicine doesn’t work. Some drugs look identical - like two white pills - but one could be 10 mg and the other 50 mg. The strength is the difference between healing and harm. Always double-check this number when you get a new bottle. If it’s changed from your last refill, ask why.
How to Take It - Clear Instructions, Not Guesswork
This part says things like “Take one tablet by mouth every 8 hours” or “Apply to skin twice daily.” It’s not just about timing. It’s about method. Does it go under your tongue? On your skin? With food? On an empty stomach? Some medications are ruined if you chew them. Others need to be taken with milk to protect your stomach. Missing these details can make the drug useless - or dangerous. If the label says “as needed,” it doesn’t mean “whenever you feel like it.” It means “only when you have the symptom it’s meant to treat.” If you’re unsure, ask your pharmacist to explain it again. Don’t assume.
Expiration Date - It’s Not Just a Suggestion
That date on the label? It’s not when the company wants you to buy a new bottle. It’s when the medicine stops being safe and effective. Most prescriptions last 12 to 18 months after being filled. After that, the chemical makeup can change. Pills might break down. Liquid antibiotics can grow bacteria. Taking expired medicine won’t always make you sick - but it might not work when you need it most. That’s why you shouldn’t keep old meds around “just in case.” If you see an expiration date that’s passed, drop it off at a pharmacy take-back program. Don’t flush it. Don’t throw it in the trash. Return it.
Prescription Number - Your Prescription’s ID
This is the Rx number. It’s usually a 5- to 7-digit code. It’s not for you - it’s for the pharmacy. But knowing it helps you when you call for refills or have questions. If you’re trying to refill online or over the phone, they’ll ask for it. It links your name to the exact prescription the doctor wrote. If you lose your label and don’t know the Rx number, you might get a delay - or worse, the wrong refill. Write it down or save it in your phone. It’s your prescription’s fingerprint.
Pharmacy and Prescriber Info - Your Safety Contacts
The label shows the pharmacy’s name, address, and phone number. It also lists your doctor’s name. These aren’t just details - they’re lifelines. If you have side effects, if you’re confused about the instructions, or if you think the label is wrong - call the pharmacy. Don’t wait. Don’t guess. Pharmacists are trained to answer these questions. They’re often more available than your doctor. And if you ever need to verify your prescription with another provider - like a specialist or ER doctor - they’ll need the prescriber’s name and contact. Keep this info handy.
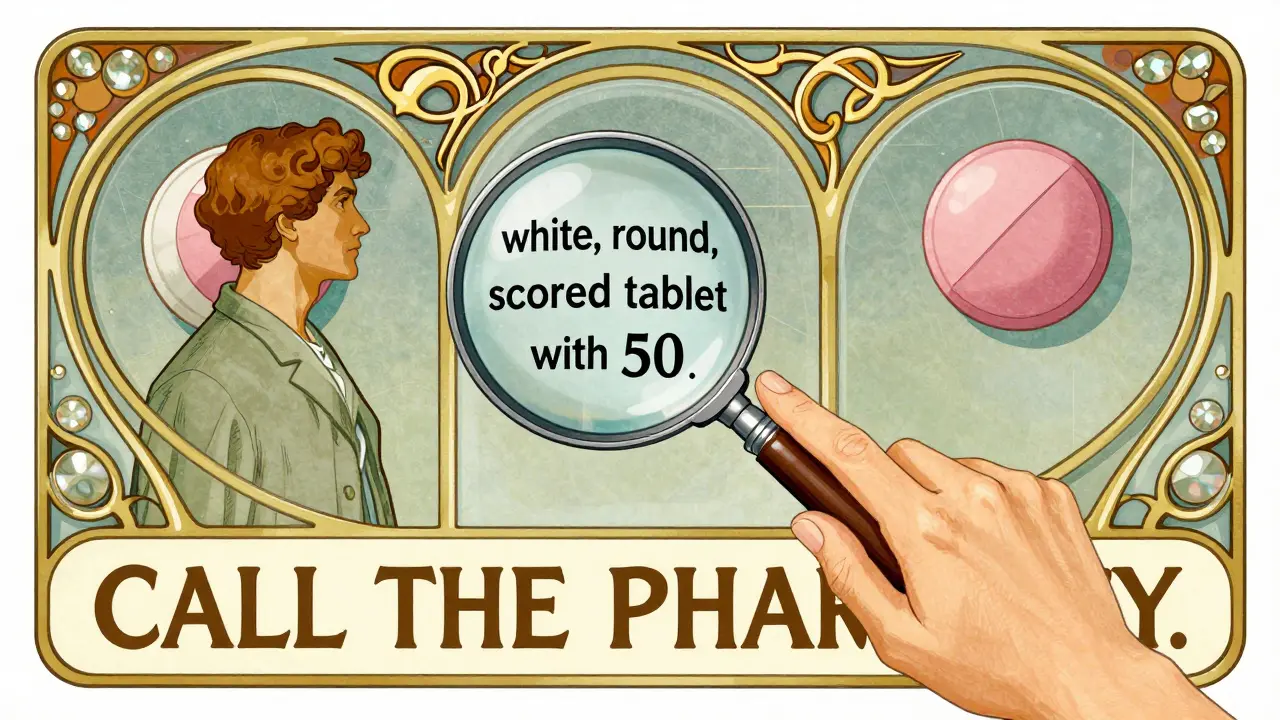
Drug Appearance - Color, Shape, Imprint
Ever opened a bottle and thought, “This doesn’t look right”? That’s because pills change. Manufacturers switch. Pills can look different even if the medicine inside is the same. That’s why the label describes the pill: “white, round, scored tablet with ‘50’ imprinted.” If your new bottle looks completely different from your last one - and the description doesn’t match - don’t take it. Call the pharmacy. This is how you catch counterfeit drugs, wrong fills, or manufacturing errors. You don’t need to memorize every pill. Just check this line every time. It’s your visual safety net.
National Drug Code (NDC) - The Universal Barcode
This is a 10- or 11-digit number, usually near the bottom. It’s not meant for you to remember - but it’s the key to tracking your medicine. Every pill, bottle, and package in the U.S. has one. It tells you who made it, what it is, and how big the package is. If there’s a recall, the FDA uses this number to find exactly which batches are affected. If you’re ever in a hospital or emergency, this number helps them identify your medication fast. You don’t need to use it daily - but knowing it exists means you can ask, “Is this the right code?” if something feels off.
Storage Instructions - Keep It Safe
Some pills need to stay cool. Others must be kept dry. Some can’t even be in the bathroom. The label might say “Store at room temperature” or “Refrigerate.” That’s not just advice - it’s science. Heat, moisture, and light can break down medicine. Insulin, for example, loses effectiveness if left out too long. Antibiotics can turn toxic. If your label says “store between 68°F and 77°F,” that’s the sweet spot. Keep it away from sunlight. Don’t leave it in your car. If you’re traveling, ask your pharmacist how to keep it safe on the go. A pill that’s gone bad might look fine - but it won’t work.
Warnings - The Red Flags You Can’t Ignore
This part might say things like “Avoid alcohol,” “May cause drowsiness,” or “Not for use in pregnancy.” These aren’t footnotes. They’re warnings. Some are printed in bold. Others are in small print - but they’re still critical. For example, if you’re taking a blood thinner and the label says “avoid NSAIDs like ibuprofen,” that’s because mixing them could cause internal bleeding. If you’re told not to drive, don’t. If it says “consult doctor if you have kidney disease,” don’t skip that step. These warnings are based on real risks - not guesswork. If you’re unsure what a warning means, ask. Don’t assume it’s minor.
Indication - Why You’re Taking It
This is the part most labels still leave out - but they shouldn’t. The indication is the reason you were prescribed the drug. “For high blood pressure.” “For depression.” “For pain after surgery.” The FDA and the United States Pharmacopeia now strongly recommend including this on every label. Why? Because people take meds for the wrong reasons. A 2022 study found that including the indication on labels reduces wrong-drug errors by 55%. Imagine someone taking insulin thinking it’s for cholesterol - that’s how mistakes happen. If your label doesn’t have this, ask your pharmacist to write it in. You have a right to know why you’re taking something.
What You Should Do Every Time You Get a Prescription
- Check your name - make sure it’s correct.
- Compare the generic name to what your doctor told you.
- Verify the dosage strength - especially if it changed.
- Read the instructions aloud. Do you understand them?
- Look at the expiration date - is it still valid?
- Check the pill’s appearance - does it match the description?
- Find the pharmacy phone number - save it in your phone.
- Ask: “What is this for?” If it’s not written, ask them to add it.
What to Do If Something Feels Off
If the label looks wrong, the pills look different, the instructions are confusing, or the name doesn’t match - don’t take it. Call the pharmacy. Ask for the pharmacist to explain it again. Use the 5 Questions to Ask About Your Prescription:
- What is the name of the medication and what is it for?
- How and when do I take it?
- What should I do if I miss a dose?
- What side effects should I expect?
- Will this interact with other meds I’m taking?
If you still feel unsure, ask for a printed handout. Many pharmacies now offer them. Or ask for a counseling session. Pharmacists are trained to help you understand - and they’re paid to make sure you’re safe.
Why This Matters - Real Consequences
One woman in California took a pill labeled for diabetes - but it was actually for seizures. She didn’t know because the indication wasn’t on the label. She ended up in the hospital. A man in Florida mixed two blood pressure drugs because he didn’t know they were the same thing under different names. He had a stroke. These aren’t rare stories. The FDA says 78% of patients don’t know why they’re taking their meds. That’s not ignorance - it’s bad labeling. And it’s fixable. The industry is changing. More labels now include the indication. More use larger fonts. More use pictograms for people with low literacy. But you still have to check. Your life depends on it.
What if my prescription label doesn’t say why I’m taking the medicine?
If the reason you’re taking the medication isn’t listed, ask your pharmacist to write it in. You have the right to know. Many pharmacies now include this, but if yours doesn’t, request it. The FDA and USP recommend it because it cuts medication errors by over half. Don’t accept vague answers like “It’s for your condition.” Ask for the specific diagnosis - like ‘high blood pressure’ or ‘depression.’
Can I still take medication after the expiration date?
Some pills might still be safe a year past expiration, but you can’t be sure. Liquid medicines, antibiotics, and insulin degrade faster and can become dangerous. Pills like aspirin or antihistamines might lose potency but rarely turn toxic. Still, the FDA doesn’t recommend using expired meds. If you’re unsure, take it to a pharmacy for disposal. They have safe drop-off programs. Never flush or throw it in the trash.
Why do some pills look different even though they’re the same medicine?
Different manufacturers make the same generic drug. They can change the color, shape, or imprint. That’s legal - but confusing. That’s why the label includes a description like “white, round, scored tablet.” Always check that description when you get a refill. If the pill looks totally different and the description doesn’t match, call the pharmacy. It could be a mistake - or a counterfeit.
What’s the difference between brand and generic names?
The brand name is what the company calls the drug - like Advil. The generic name is the active ingredient - ibuprofen. Generics are cheaper and work the same way. But if you don’t know the generic name, you might accidentally take two versions of the same drug - like buying both Advil and a store-brand ibuprofen. That’s how you overdose. Always check the generic name on your label.
Can I trust the label if my doctor told me something different?
The label is the official, FDA-approved instruction. If your doctor told you something different - like “take twice a day” when the label says “once a day” - ask your pharmacist to clarify. Sometimes, doctors adjust doses based on your needs. But the label must match what’s legally approved. Never change your dose without talking to your doctor or pharmacist. If there’s a conflict, call the pharmacy. They’ll verify with the prescriber.

10 Comments
I used to ignore labels until my mom had a bad reaction to a generic swap. She didn’t know the active ingredient was the same as her old med, but the dosage was different. I wish more people knew how much this stuff matters. It’s not just paperwork-it’s survival.
Now I check every single thing when I pick up a script. Name? Check. Strength? Check. Appearance? Double-check. And I always ask, ‘What’s this for?’ Even if it’s written. You never know when the pharmacist made a note you didn’t see.
Pharmacists are the real MVPs here. They’re the ones catching mistakes before they happen. We treat them like order-takers, but they’re the last line of defense.
Also-please, please, please don’t keep expired meds. I found my grandma’s 10-year-old antibiotics in her bathroom cabinet. I threw them out. She was mad. But I’d rather be the bad guy than the one who says, ‘I told you so’ after she ends up in the ER.
It is imperative that patients be educated regarding the critical importance of pharmaceutical labeling compliance. The statistical prevalence of medication errors-approximately 1.5 million annually in the United States-is not merely an epidemiological concern; it is a systemic failure of patient literacy and institutional communication.
One must recognize that the inclusion of the indication on prescription labels is not merely a recommendation, but a bioethical imperative. The United States Pharmacopeia, in conjunction with the Food and Drug Administration, has demonstrated through empirical research that the omission of therapeutic intent correlates directly with increased morbidity and mortality.
It is therefore the duty of every healthcare stakeholder-pharmacists, prescribers, and patients alike-to advocate for standardized, legible, and comprehensive labeling. The cost of noncompliance is measured not in dollars, but in lives.
Let’s be real-the whole system is a regulatory theater. You think your NDC code matters? Nah. Big Pharma just uses it to track which batch got recalled after they cut corners. The real danger? The fact that generics are manufactured in overseas facilities with zero transparency.
And don’t get me started on ‘expiration dates.’ That’s just a profit-driven expiration window. Studies show 80% of meds are still potent 5+ years out. The FDA knows this. They just want you to repurchase. It’s capitalism disguised as safety.
Also-why do you think they make pills look different? To confuse you into thinking you got a counterfeit. It’s psychological control. You’re being conditioned to distrust your own perception. Wake up.
And the ‘storage instructions’? Pure marketing. Insulin doesn’t ‘lose potency’ if left out for 12 hours-it’s just a scare tactic to sell coolers. I’ve been storing mine in my glove compartment for years. Still works. Just saying.
Okay, so I just read this whole thing… and I’m not even gonna lie-I think this is a government mind-control scheme. Like, why is EVERYTHING on the label? Why do they need my name, my doctor’s phone number, the NDC, the imprint, the storage temp… it’s like they’re building a dossier on me.
And what if… what if the pharmacy’s phone number is a trap? What if they’re recording every call? What if the ‘expiration date’ is actually a tracker? I Googled it-there’s a Reddit thread from 2018 where someone said the NDC code has GPS embedded in it. I didn’t believe it… until I saw the font. It’s the same font they use in the CDC’s ‘vaccine compliance’ PDFs.
Also-why does the label say ‘Do not take with alcohol’? Because they want you to think you’re safe… but what if the real danger is the *label itself*? What if it’s laced with something? I think I’m being watched.
…I’m gonna call my pharmacist. Just in case.
…I’m scared.
…I’m calling my mom.
…I’m moving to Canada.
My pharmacist always says, ‘If you’re unsure, ask.’ So I do. And they’re always happy to explain. It’s not that hard. Just take a second. You’re worth it.
This is one of those posts that should be handed out with every first prescription. Seriously. I teach high school health, and I’m stealing this to use in class next week.
One of my students had to switch from brand to generic Adderall last year. She thought she was getting a weaker version because the pill was a different color. She stopped taking it for two weeks and her anxiety spiked. If she’d read the label’s description-‘yellow, oval, scored tablet with ‘A10’’-she’d have known it was the same thing.
We need to teach this stuff early. Not just ‘take your meds’-but ‘know your meds.’ It’s not just health literacy. It’s self-advocacy.
OMG I just read this and I am so happy because in India we have this problem too but even worse!! Like my cousin took diabetes medicine and it was labeled as blood pressure and she took it for 3 days and almost died!! And no one told her why!! And the pharmacy guy just laughed and said 'its same thing no?'!! I mean seriously??
And also the pills in India look totally different every time!! One time it was blue next time it was white and I was like 'are you sure this is same?' and they said 'yes yes' and I was like 'but the imprint is different!!' and they said 'oh that is new design'!!
And expiration date?? We use medicine after 3 years!! My grandma says 'if it looks fine then it is fine'!! I think this post is so important for India too!! We need to teach this in schools!!
Also I think the government should make all labels in Hindi and English and also with pictures!! Like a heart for blood pressure and a brain for depression!! So even if you cant read you know!!
And why dont they put the doctors name in big letters?? I mean its so small!! I think they are hiding something!!
And I think the NDC code should be on the bottle in QR code so we can scan and see everything!!
And also why dont they make the font bigger?? I have bad eyes!!
Also I think the pharmacy should give us a free consultation every time!!
And I think all this should be mandatory!!
Also I think this should be on TV!!
Also I think I should send this to my cousin!!
Also I think I should post this on WhatsApp group!!
Also I think I should call my MP!!
Also I think I should write a letter to WHO!!
Also I think I should start a movement!!
Also I think I should write a book!!
Also I think I should go to med school!!
Also I think I should stop typing now!!
Just wanted to say I used to be one of those people who never checked the label… until I accidentally took my husband’s blood thinner because the pills looked the same. He’s fine, but I spent three days in the hospital. Don’t be like me.
Now I take a pic of the label every time I get a refill. Seriously. I have a folder on my phone called ‘Medication Log.’ I even write down the Rx number. It’s weird… but I’m alive.
Also-side note: if the label says ‘take with food’ and you’re hungry, just eat a cracker. Don’t overthink it. But if you’re not hungry? Don’t force it. The ‘with food’ thing is mostly to protect your stomach, not to make you snack.
Wow. Just… wow. You’d think after all these years, people would know this stuff. I mean, come on. This isn’t rocket science. It’s a label. It’s not a mystery novel. You don’t need a PhD to read ‘Take one tablet daily.’
And yet… here we are. People are dying because they didn’t look at the generic name. Because they didn’t check the expiration. Because they thought ‘as needed’ meant ‘whenever I feel like it.’
It’s not complicated. It’s not confusing. It’s just… laziness. And entitlement. And ignorance. And I’m tired of cleaning up the mess.
Stop being passive. Read the damn label. Or don’t take the pill. Either way, don’t blame the pharmacist when you’re the one who didn’t care enough to look.
I’ve been on a dozen different meds over the last 10 years. And you know what I’ve learned? The label is the only thing that never lies.
Doctors change their minds. Pharmacies mix up bottles. Online pharmacies send the wrong thing. Insurance switches generics. Manufacturers change pill shapes. Insurance companies push cheaper versions. Your body changes. Your tolerance changes.
But the label? It’s printed. It’s official. It’s the last static thing in a world of chaos.
I used to think I knew what I was taking. Then I missed a dose once because I thought the pill looked ‘off’-and I was right. It was a different generic. I called. They apologized. They gave me a free refill.
Now I don’t just read the label. I *reverence* it. It’s my anchor. My rulebook. My silent guardian.
And if you’re not doing the same? You’re playing Russian roulette with your health. And that’s not bravery. It’s just… dumb.